Genetics-related juvenile recurrent parotitis of identical twin: a case report
Introduction
JRP is caused by intricate factors. Some suggested contributory factors to the development of the condition are congenital ductal malformation (1,2), genetic factors (3,4), viral or bacterial infection, IgA (5), IgG deficiency and local manifestation of an autoimmune disease (6,7). In summary, the pathogenesis of juvenile recurrent parotitis (JRP) remains unclear. Children often have a history of mumps or contacting patients who have mumps before onset. Swelling and/or pain in JRP are localized in the parotid gland (8). The clinical characteristic is unilateral or bilateral swelling of parotid gland, which is usually not synchronous and suppurative (9).
Although JRP is self-limited and may completely regress after puberty, pediatricians should be aware of the cause of this disease and should be able to diagnose and treat it (10). A minority of JRP patients cannot be healed after puberty, even if puberty ends spontaneously. In some cases, the symptoms of JRP remain until adulthood.
In our study, two identical twins were diagnosed with JRP. Their mother also claimed that she had the same diagnosis during childhood. We suspect that the occurrence of this disease in these twins may have resulted from genetic factors.
Case presentation
Two 4-year-old identical male twins (Y and F) suffered from recurrent swelling on their unilateral or bilateral faces for approximately 14 days. Both had almost the same symptoms, which were meticulously noted every month. The swelling was associated with pain in the parotid gland and a salty taste in their mouths. Past medical history included otitis media and recurrent episodes of parotitis since age 3 years, most often in single glands and occasionally in both glands. The attacks occurred approximately 6 times before the current presentation, and each attack lasted approximately five days. These events had been treated with oral amoxicillin or other antibiotic prescriptions, usually with rapid clinical improvement. However, the symptoms relapsed after a period of time, resulting in their referral to our hospital.
Physical examination of Y revealed a generally normal physical condition. On extraoral examination, there was an obviously diffuse swelling at the front of the ear and the subauricular regions of the right parotid gland. A tender and erythematous swelling was observed at the right parotid gland; this was slightly firm and warm on palpation. The right submandibular lymph nodes were slightly firm in consistency. A small amount of gelatinous secretion was extruded from the right parotid duct. Slight inflammation and tenderness were observed over the right duct opening. On extraoral examination of F, there was an obvious diffuse swelling at the bilateral parotid glands. On palpation, there was a slightly firm consistency. The skin temperature was somewhat high, and there was tenderness on palpation; tenderness of the submandibular lymph nodes was noted. Some secretion was extruded from the left and right parotid ducts, and there was no inflammation or tenderness over the duct openings. Both boys had a fever of approximately 38.5 °C at the beginning of the attack, and they both had a history of mumps.
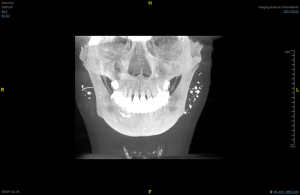
The complete blood picture of F and Y was showed in Table 1. Ultrasonogram of the left parotid gland of F revealed multiple hypoechoic areas and a heterogeneous distribution of internal echoes suggestive of inflammatory changes and dilation of acini in the left parotid gland. Blood flow was richer in the left than in the right parotid gland. An ultrasonogram also showed multiple oval hypoechoic areas, and the blood flow signal shown in the CDFI revealed bilateral cervical lymph node enlargement. However, Y did not have ultrasonography at our hospital. Both had parotid sialography. The terminal ducts showed areas of ‘blobs’ and ‘dots’ of contrast media indicating sialectasis (Figure 1).
Table 1
| Characteristics | F | Y | Normal |
|---|---|---|---|
| WBC (×109/L) | 6.0 | 5.2 | 3.5–9.5 |
| Hemoglobin (g/L) | 126 | 132 | 130–175 |
| Red blood cell volume | 0.328 | 0.420 | 0.4–0.5 |
| Mean corpuscular volume (fl) | 80.4 | 90 | 82–100 |
| Mean corpuscular hemoglobin (pg) | 26.5 | 30.5 | 27–34 |
| Lymphocyte percent (%) | 52.1 | 53.2 | 20–50 |
| ESR (mm/h) | 2 | 2 | 0–15 |
| CRP (mg/L) | 2.81 | 2.69 | 0–10 |
| Serum amylase (U/L) | 92 | 89 | 25–115 |
| IgG (mg/dL) | 992 | 874 | 504–1,464 |
| IgA (mg/dL) | 67 | 123 | 27–195 |
| IgM (mg/dL) | 91 | 82 | 24–210 |
| IgE (IU/mL) | 27.7 | 25.6 | 0–100 |
WBC, white blood cell; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein.

Based on the history given by the patients, the clinical picture, laboratory investigations, ultrasonogram appearance and sialographic appearance, a final diagnosis of JRP was given. As there was little secretion or gelatinous secretion from the ducts, pilocarpine (2 mg per administration, 2 times a day) was advised to alleviate the patients’ symptoms. In addition to pilocarpine, attention to good oral hygiene, massage of the parotid gland, warmth, use of chewing gum and lemonade may be helpful in reducing the attack frequency (11). The patients were also advised to keep a record of the frequency and duration of the symptoms and signs of this disease. Half a month later, they came to the hospital for a
The treatment seemed to be effective as there was just one recurrence during the 7 months’ follow-up. At the latest subsequent visit, cetylpyridinium chloride buccal tablets (one pill at a time) were suggested for use when the parotid gland flared up.
Family history
The twins’ father denied a history of parotitis, while their mother, a 37-year-old woman, presented with a complaint of swelling on the left side of the face for 7 days, also had JRP when she was a child. The swelling was associated with pain, discomfort and a salty taste in her mouth. The first attack happened at 14 years of age, and there were two attacks before this current attack. In the general physical examination, she had diabetes and a fatty liver. On extraoral examination, there was obvious diffuse swelling in the left parotid gland. A small amount of secretion extruded from the left parotid duct. The cause of this attack may have been fatigue. She said that she had a history of xerostomia for approximately the previous 5 years. However, she did not have a history of mumps.
The complete blood count of their mother was showed in Table 2. The levels of complement (C3, C4), antinuclear antibodies, anti-Ro and La, rheumatoid factor, antithyroid antibodies, thyroxine and thyroid stimulating hormone were within normal limits. Minor salivary gland biopsy of the lower lip showed no focal aggregates of lymphocytes in the parenchymal lobules of the salivary tissue. These findings ruled out an underlying autoimmune disease, such as Sjogren syndrome. The radiological investigation of choice for confirmation of a diagnosis of JRP, sialography, was completed. Terminal ducts also showed areas of ‘blobs’ and ‘dots’ of contrast media indicating sialectasis (Figure 2).
Table 2
| Characteristics | Mother | Normal |
|---|---|---|
| WBC (×109/L) | 7.1 | 3.5–9.5 |
| Monocytes (%) | 3.7 | 3–10 |
| Neutrophils (%) | 70.1 | 40–75 |
| IgG (g/L) | 16.9 | 7–16 |
| IgA (g/L) | 5.18 | 0.7–4 |
| IgM (g/L) | 1.79 | 0.4–23 |
| IgE (IU/mL) | 33.4 | 0–100 |
WBC, white blood cell.
Discussion
JRP is a rare inflammatory salivary gland disease of childhood after mumps (12). It presents clinically in the form of unilateral or bilateral swelling of the parotid gland, is usually followed by fever and general malaise and is characterized by recurrent nonsuppurative parotitis, spontaneously evolving towards parotid gland dysfunction (9). Even though a variety of factors are thought to cause JRP, including genetic and immune factors, infection, dehydration, allergy, ductal abnormality, and ductal obstruction, most authors favor a multifactorial cause (13). Although JRP is a self-resolving disease and can completely regress after puberty, it is also important to know how to recognize and diagnose JRP for early treatment because of the risk of significant destruction of the glandular parenchyma. The most pathognomonic sign of JRP is wide opening of Stensen’s papilla with plaque exudates. A firm mass can be felt when the symptomatic gland is palpated (14). In addition to the clinical manifestations, laboratory findings are also essential, including laboratory examination, ultrasonography, and parotid sialography.
This study presented two twin boys, 4 years old, who were diagnosed with JRP. Because of their premature delivery, similar to their mother, and their fussy eating, their physical condition was fair and they developed fever easily. Previously, they had been seen by a doctor for chronic otitis media when they were 2 years old. The swollen parotid gland was mostly accompanied by a fever of approximately 38.5 °C, sometimes accompanied by pharyngitis or respiratory tract infection. Their parents denied any other family history. The twin boys had a habit of not brushing their teeth at night. Interestingly, their mother also had a history of JRP when she was a child that had now become adult recurrent parotitis, which suggested that genetic factors were involved in this case (14).
From his laboratory examination, F had a lower IgA, which should highlight this abnormal phenomenon. Because IgA is the most common immune deficiency, a coincidental association between IgA deficiency and recurrent parotitis is possible. There was a study speculated that a lack of IgA in the parotid gland may be associated with an inability to completely clear inflammatory stimuli. This, in turn, may subsequently lower the threshold for developing inflammatory pathology. Thus, in some cases, it can be speculated that IgA deficiency may play a role in the pathophysiology of recurrent inflammation of the salivary gland (5). The most frequently used testing for the diagnosis of JRP is still sialography, which is a hallmark in the diagnosis of JRP (1,15). Ultrasonography and magnetic resonance imaging-sialography are noninvasive and have been increasingly used for diagnosis and during follow-up (7). Currently, ultrasound has evolved as a standard component of salivary gland assessment, and sialography may complement imaging with ultrasound (or CT, as in this case) to offer the highest acuity definition of the salivary ducts (15). Sialography was performed not only for diagnostic purposes but also for gland lavage, which helped to clear the mucus plug or cellular debris.
The treatment is based on the diagnosis and clinical symptoms and signs. Stopping recurrent infection of the glands is the purpose of the treatment and prevents irreversible damage to the parotid glands. In the acute stage of JRP, antibiotics can be used for treatment, especially for Staphylococcus and Streptococcus (4). If there is almost no secretion or gelatinous secretion from the parotid duct at the first visit, antibiotics are not needed. In addition, other methods are used to treat JRP, including chewing gum, drinking lemonade, massaging the parotid gland, duct probing and dilation, hot compresses on the parotid gland and so on, to increase salivary flow, which has been found to be helpful in alleviating the symptoms. Other treatment methods described in the literature are invasive and are now almost abandoned, such as duct ligation, parotidectomy and tympanic neurectomy (16). Studies have shown that a certain degree of stimulation can promote the secretion of saliva and spur the development of glands (17). At present, a certain degree of stimulation is suggested to stimulate the glands of JRP patients, including chewing gum, taking vitamin C, a small dose of pilocarpine and so on. In this case, at their first follow-up, Y had a small amount of pus from the right parotid duct when pressing the parotid gland; therefore, cefdinir dispersion tablets (antibiotics) were first recommended for use to alleviate the symptoms. Antibiotic treatment aims to prevent additional damage from the glandular parenchyma to alleviate the symptoms (6,18). JRP is a self-limiting disease, and most of the cases resolve by puberty; the symptoms usually subside, and the disease may resolve completely (11), so treatment of the condition should be conservative. However, if the inflammation occurs recurrently and affects the normal life of children, the method of intraductal irrigation can be used. Studies have shown that salivary gland endoscopy is an option for the treatment of recurrent mumps in adolescents, which is helpful for diagnosis and treatment intervention, allowing intraductal irrigation and dilation of stenosis (19). There was no significant difference in the effect of lavage with normal saline, hydrocortisone, antibiotics or a combination of these solutions. Sialography seems to be an option for diagnosis and treatment, although it has not been shown to be more effective than simple irrigation. All the rinses seem effective (4,9).
Conclusions
In summary, a variety of factors have been proposed for JRP. In this study, two twin boys and their mother, who all had JRP, may be the argument for a genetic cause. Dentists should be fully aware of this disease and have enough knowledge of how to diagnose and treat it. Owing to the patients with this disease being juveniles, parents play an important role during the course of the disease.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundation of China (Grant No. 81671004, 81771089, 81800990), Natural Science Foundation of Shanghai (Grant No. 16ZR1419000), Shanghai Jiao Tong University Biomedical Engineering cross research foundation (YG2015MS03), Shanghai Summit & Plateau Disciplines.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.org/article/view/10.21037/fomm.2020.03.04/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rosbe KW, Milev D, Chang JL. Effectiveness and costs of sialendoscopy in pediatric patients with salivary gland disorders. Laryngoscope 2015;125:2805-9. [Crossref] [PubMed]
- Wittekindt C, Jungehulsing M, Fischbach R, et al. HNO 2000;48:221-5. [Chronic recurrent parotitis in childhood in monozygotic twins Magnetic resonance sialography]. [Crossref] [PubMed]
- Reid E, Douglas F, Crow Y, et al. Autosomal dominant juvenile recurrent parotitis. J Med Genet 1998;35:417-9. [Crossref] [PubMed]
- Iro H, Zenk J. Salivary gland diseases in children. GMS Curr Top Otorhinolaryngol Head Neck Surg 2014;13:Doc06. [PubMed]
- Fazekas T, Wiesbauer P, Schroth B, et al. Selective IgA deficiency in children with recurrent parotitis of childhood. Pediatr Infect Dis J 2005;24:461-2. [Crossref] [PubMed]
- Adeboye SO, Macleod I. Recurrent Parotitis of Childhood or Juvenile Recurrent Parotitis – A Review and Report of Two Cases. Dent Update 2014;41:73-6. [Crossref] [PubMed]
- Leerdam CM, Martin H, Isaacs D. Recurrent parotitis of childhood. J Paediatr Child Health 2005;41:631-4. [Crossref] [PubMed]
- Nahlieli O, Shacham R, Shlesinger M, et al. Juvenile Recurrent Parotitis: A New Method of Diagnosis and Treatment. Pediatrics 2004;114:9-12. [Crossref] [PubMed]
- Berta E, Angel G, Lagarde F, et al. Role of sialendoscopy in juvenile recurrent parotitis (JRP). Eur Ann Otorhinolaryngol Head Neck Dis 2017;134:405-7. [Crossref] [PubMed]
- Xie LS, Pu YP, Zheng LY, et al. Function of the parotid gland in juvenile recurrent parotitis: a case series. Br J Oral Maxillofac Surg 2016;54:270-4. [Crossref] [PubMed]
- Garavello W, Redaelli M, Galluzzi F, et al. Juvenile recurrent parotitis: A systematic review of treatment studies. Int J Pediatr Otorhinolaryngol 2018;112:151-7. [Crossref] [PubMed]
- Gadodia A, Seith A, Sharma R, et al. MRI and MR sialography of juvenile recurrent parotitis. Pediatr Radiol 2010;40:1405-10. [Crossref] [PubMed]
- Francis CL, Larsen CG. Pediatric sialadenitis. Otolaryngol Clin North Am 2014;47:763-78. [Crossref] [PubMed]
- Sujatha S, Rakesh N, Raghav N, et al. Case report: Report of a rare case of juvenile recurrent parotitis and review of literature. Eur Arch Paediatr Dent 2009;10:31-4. [Crossref] [PubMed]
- Carta F, Farneti P, Cantore S, et al. Sialendoscopy for salivary stones: principles, technical skills and therapeutic experience. Acta Otorhinolaryngol Ital 2017;37:102-12. [PubMed]
- Shacham R, Droma EB, London D, et al. Long-term experience with endoscopic diagnosis and treatment of juvenile recurrent parotitis. J Oral Maxillofac Surg 2009;67:162-7. [Crossref] [PubMed]
- Wu S, Wang B, Yu C, et al. Juvenile recurrent parotitis: Soft foods contribute to the delayed development of salivary glands. J Oral Rehabil 2020;47:485-93. [Crossref] [PubMed]
- Shkalim V, Monselise Y, Mosseri R, et al. Recurrent parotitis in selective IgA deficiency. Pediatr Allergy Immunol 2004;15:281-3. [Crossref] [PubMed]
- Schneider H, Koch M, Kunzel J, et al. Juvenile recurrent parotitis: a retrospective comparison of sialendoscopy versus conservative therapy. Laryngoscope 2014;124:451-5. [Crossref] [PubMed]
Cite this article as: Ye L, Shi H, Yu CQ, Zheng LY. Genetics-related juvenile recurrent parotitis of identical twin: a case report. Front Oral Maxillofac Med 2020;2:6.