
The impact of volume and surgical throughput on outcomes in head and neck reconstruction: a systematic review
Introduction
Microvascular free tissue transfer is the gold standard of head and neck (H&N) reconstruction. Surgical techniques around free flap surgery have evolved enormously over the last few decades; we now live in the era of patient-specific 3D-aided H&N free flap reconstruction (1,2).
The general belief is that this kind of complex surgery should be carried out in high volume centers, with high numbers of cases/surgical throughput, in order to achieve the best possible outcomes for the patients. Many other factors favoring H&N centralization have been cited, including teaching, education, training, cost reduction and efficient health economy, teamwork building, research, audit and governance monitoring (3). In reality, most of these benefits can be achieved anywhere, without centralization of services, as long as clinical outcomes are favorable for patients. Other proposals to improve outcomes (such as dual attending surgeon operating, minimize junior doctors operating) are yet to prove their efficiency (4).
Literature from other specialties suggests that the relationship between volume and outcomes is not always linear, but often follows a bell distribution. This of course means that outcomes might improve up to a certain volume level, after which any further increase has a detrimental effect (5). On other occasions, achievement of acceptable outcomes might plateau after a certain case volume and remain unchanged thereof (6).
Recent systematic reviews and meta-analyses suggest an acceptable average free flap success level for H&N reconstruction of 95% (7). This is somehow lower than breast and limb reconstruction (8), which can partly be explained by the general fitness and performance score of the H&N patients. Taking into account salvage cases and ORN cases, one can safely consider a free flap success rate of over 90% as the minimum acceptable outcome in H&N reconstruction.
Unfortunately, free flap outcomes reporting isn’t universally mandatory. In the UK, the UKNFR registry is a step towards the right direction (9), but until it becomes a practice requirement, the scene of the free flap H&N reconstruction will remain vague at best.
Here, I conduct a systematic review of all available published evidence, in an attempt to establish a correlation between surgical throughput and clinical outcomes in H&N free flap reconstruction. I discuss the pitfalls of data collection and reporting, and I debate the pros and cons of centralization of H&N services. I present the following article in accordance with the PRISMA reporting checklist (available at https://fomm.amegroups.com/article/view/10.21037/fomm-20-60/rc).
Methods
Protocol and registration
I performed a systematic review of all available literature in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and the guidance set out by the Cochrane Handbook of Systematic Reviews of Intervention (10,11). The systematic review was submitted to the International Prospective Register of Systematic Reviews (PROSPERO) (CRD206975).
Eligibility criteria
Study designs and report characteristics
All human experimental (randomized control trials and trials) and observational studies (case series, case reports, case control and cohort) were eligible for inclusion. There was no limitation on the sample size. Review papers and eligible studies were screened for papers not detected by the search algorithm. Animal studies were excluded. Language was restricted to English literature.
Participants
All adult (over 18 years) patients undergoing H&N autologous free tissue transfer were included. There were no limitations on the type of flap or reconstruction indication (tumor ablation, ORN, etc.) however trauma cases were excluded.
Interventions
I included all publications reporting surgical outcomes in H&N free flap reconstruction whilst offering information about the institutional volume/number of cases/surgical throughput. I accepted reports comparing outcomes from the same institute but different time periods (thus indicating a change in numbers treated vs. outcomes). I have also included multicenter studies where the comparison between units was clearly made based on volume/number of cases.
Comparators
Any study that directly reported and/or compared surgical outcomes in H&N free flap reconstruction with total number of treated patients was included. The treating units were classified as large (>50 cases/year) based on the BAHNO recommendations for double team consultant operating and recommended volume per consultant (12). Even if this direct comparison wasn’t made, I attempted to extract this information from the available data and documented whether this was unclear or impossible based on the available information.
Outcomes and definitions
The primary outcome was free flap success rate (N/%). Flap failure was defined as a non-surviving free flap, requiring debridement and/or removal, and/or further reconstruction (further free flap and/or further pedicled flap and/or further dressing).
Secondary outcomes included:
- Perioperative mortality (30 days);
- Clavien-Dindho grade III–IV complications;
- 28-day unplanned hospital re-admission;
- Return to theatre for exploration and flap salvage.
Information sources and search strategy
I performed a comprehensive literature review using the advanced search in MEDLINE (OVID interface), EMBASE (OVID interface), and PubMed from its origin till August 2020.
The following terms (MeSH) were used: “microvascular free tissue transfer” OR “free flap” OR “head and neck reconstruction” AND “number” OR “outcomes” OR “free flap salvage” OR “success rate”. Each term was exploded prior to being combined. Initial results were screened based on titles and abstracts. The references of all eligible papers were screened, and any missed studies were included. If unable to extract data from the literature, I contacted the corresponding author. If there was no response, the study was excluded, and documented in the PRISMA flow chart below. I also screened ClinicalTrials.gov for any ongoing trials.
Data extraction and management
All data extracted were tabulated in a predefined sheet. I recorded the type of study, number of flaps, type of flap used, number of cases per year in that particular institute, and all the primary and secondary outcomes.
Quality assessment
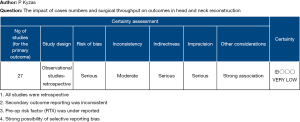
I assessed for publication bias as previously described (13). The quality of evidence was assessed by the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach.
Statistical analysis
I aimed to record the free flap success rate (%) in all included studies and compare it to the number of cases performed per year within the same institution or team (denominator). Should data quality allowed, I aimed to calculate the relative risk ratios with 95% confidence intervals using the Cochran-Mantel-Haenszel test. I expected significant between-study heterogeneity; therefore, a random-effects model was applied. Heterogeneity was measured using the I2 statistic (claiming significance at P<0.05). Publication bias was assessed using the established funnel plot method.
Results
PRISMA flow diagram (Figure 1)
My initial search strategy generated a large volume of titles [2,134]. After screening for duplicates, titles and abstracts, I analyzed 52 full text articles. Twenty-five were excluded, including two reviews, 7 with overlapping data, 8 with selective presentation of data, 5 with no available data at all and 3 non-English literature papers. Therefore, a total of 27 articles were included and fully assessed.
Primary outcome (Table 1)
Table 1
| Study | Country/ region/area |
Total number flaps | Time period | Number cases/year | Large unit (yes/no) | Types of flap | Flap success rate | Post RTX | Grade certainty |
|---|---|---|---|---|---|---|---|---|---|
| Al-Dam, J Craniomaxillofac Surg, 2014 (14) | Germany | 103 | 2011–2012 | 103 | Yes | Fibula, RFF, LD, ALT, DCIA, Scapula, MSAP | 98/103 (95.15%) | 23 (24.4%) | Low |
| Spoerl, Oral Maxillofac Surg, 2020 (15) | Germany | 494 | 2009–2018 | 50 | Yes | Fibula, RFF, LD, ALT, DCIA, Scapula, MSAP, lateral arm, pec major | 443/494 (90%) | 129 (26%) | Low |
| Marttila, Br J Oral Maxillofac Surg, 2018 (16) | Finland | 191 | 2005–2010 | 38 | No | RFF, ALT, DCIA, Scapula, Rectus, Fibula | 181/191 (95%) | 0 (0%) | Very low |
| Kovatch, Laryngoscope, 2019 (4) | USA | NA | NA | Mean 83 | Yes | All types | 95.7% (reported) | NA | Very low |
| Kessler, J Craniomaxillofac Surg, 2012 (17) | Netherlands | 81 | 2007–2011 | Mean 20 | No | RFF, Fibula, ALT, Scapula | 100% | 0 (0%) | Low |
| Rendenbach, Int J Oral Maxillofac Surg, 2018 (18) | Europe | NA | NA | NA | Mixture of units | All types | Majority over 90%. Authors mention no difference between centres or specialties | NA | Moderate |
| Salama, Int J Oral Maxillofac Surg, 2009 (19) | USA | 71 | 2002–2005 | 23 | No | RFFF, Fibula ALT, rectus | 67/71 (94%) | 0 (0%) | Low |
| Eckardt, J Craniomaxillofac Surg, 2003 (20) | Germany | 500 | 1982–2000 | 28 | No | Jejunum, RFFF, Scapula, LD, Fibula, Gracilis, Rectus, DCIA, Lat Arm | 470/500 (94%) | Unclear but less than 10% | Low |
| Pohlenz, Int J Oral Maxillofac Surg, 2012 (21) | Germany | 1,000 | 1987–2010 | 75 | Yes | LD, RFFF, ALT, Fibula, DCIA, Jejunu | 870/100 (92.4%) | NA | Very low |
| Lou, Int J Oral Maxillofac Surg, 2019 (22) | China | 1,038 | 2006–2017 | 103 | Yes | Fibula, DCIA, Scapula | 1,024 (99%) | 187 (18%) | Very low |
| Wang, Br J Oral Maxillofac Surg, 2018 (23) | China | 169 | 2011–2016 | 33 | No | RFFF | 168 (99%) | 8 (3.5%) | Low |
| Sugiyama, Head Neck, 2016 (24) | Japan | 773 | 1995–2006 | 35 | No | Jejunum | 750 (97%) | 218 (29.5%) | Low |
| Nouraei, J Plast Reconstr Aesthet Surg, 2015 (25) | UK | 11,841 | 2003–2013 | 118 | Mixture of units | All flaps | 11,345 (95%) | Unclear | Very low |
| Ho, Br J Oral Maxillofac Surg, 2012 (26) | UK | 1,278 | 1992–2009 | 70 | Yes | All flaps | 1,214 (96%) | Unclear | Moderate |
| Sweeny, Laryngoscope, 2020 (27) | USA | 2,890 | 2007–2017 | 280 | Mixture of units | All flaps | 2,757 (95.1%) | Unclear | Low |
| Weckx, Oral Surg Oral Med Oral Pathol Oral Radiol, 2017 (28) | Belgium | 100 | 2011–2015 | 25 | No | ALT, Fibula | 96 (96%) | NA | Very low |
| Klosterman, Otolaryngol Head neck Surg, 2015 (29) | USA | 136 | 1993–2013 | 8 | No | RFF, Fibula | 124 (92.6%) | NA | Low |
| Liang, Br J Otorhinolaryngol, 2018 (30) | Brazil | 98 | 2007–2015 | 12 | No | RFF, Fibula, ALT, Jejunum | 75 (90%) | NA | Very low |
| Zhang, Int J Oral Maxillofac Surg, 2015 (31) | Taiwan | 4,640 | 1979–2013 | 136 | Yes | All flaps | 4404 (97%) | 139 (3.1%) | Moderate |
| Farquhar, Otolaryngol Head Neck Surg, 2018 (32) | USA | 170 | 2007–2014 | 25 | No | NA | 151 (89%) | NA | Low |
| Brady, Am J Otolaryngol, 2017 (33) | USA | 1,417 | 2015–2013 | 170 | Yes | All flaps | Data for 582 (95%) | NA | Moderate |
| Thomas, JAMA Facial Plast Surg, 2018 (34) | USA | 1,115 | 2012–2014 | Multiple centres | Mixture of units | All flaps | Unclear | NA | Moderate |
| Kucur, Eur Arch Otorhinolaryngol, 2016 (35) | USA | 260 | 2006–2010 | 65 | Yes | All flaps | 249 (96.5%) | NA | Low |
| Husso, J Reconstr Microsurg, 2016 (36) | Finland | 594 | 1995–2012 | 33 | No | All flaps | 578 (97%) | NA | Moderate |
| Smith, Br J Oral Maxillofac Surg, 2005 (37) | Aystralia | 263 | 1987–2002 | 18 | No | RFFF | 254 (96.6%) | NA | Very low |
| Dassonville, Eur Arch Otorhinolaryngol, 2008 (38) | France | 213 | 2000–2004 | 52 | Yes | RFFF, Fibula, Scapula | 1,999 (93.4%) | Unclear | Low |
| Ross, J Reconstr Microsurg, 2008 (39) | UK | 584 | 1993–2003 | 58 | Yes | All flaps | 550 (94%) | Unclear | Moderate |
RFF, radial forearm flap; LD, latissimus dorsi flap; ALT, anterolateral thigh flap; DCIA, deep circumflex iliac artery flap; MSAP, medial sural artery perforator flap; RFFF, radial forearm free flaps; NA, not applicable.
All 27 papers were retrospective case series (Table 1). There were no randomized controlled trials. Eleven articles came from low volume centers, 12 from high volume centers and 4 were multicenter studies including both high and low volume units. The number of H&N flaps/year ranged from 8 to 280. The reported free flap success rate ranged from 89% to 100% (with the vast majority of studies reporting results between 93–96%). There was no association between unit volume and free flap success rate; this was further emphasized in the 4 studies presenting results from various centers. All studies but two have used a variety of free flaps. Only 8 studies provided data on pre-op radiotherapy. Data synthesis was unnecessary as all studies reported overlapping outcomes.
Secondary outcomes (Table 2)
Table 2
| Study | Mortality | Index side of cancer | Readmissions (%) | Return to theatre (%) | Clavien III–IV |
|---|---|---|---|---|---|
| Al-Dam, J Craniomaxillofac Surg, 2014 (14) | 4 (3.8%) | Oral | NA | 24 (23.3%) | Not mentioned but over 25% |
| Spoerl, Oral Maxillofac Surg, 2020 (15) | NA | Oral (91%); extraoral (9%) | NA | 51 (10%) | Not mentioned but over 30% |
| Marttila, Br J Oral Maxillofac Surg, 2018 (16) | 0 (0%) | Oral | 14 (7%) | 48 (25%) | 20 (12%) |
| Kovatch, Laryngoscope, 2019 (4) | NA | All H&N | NA | NA | 7.5% (mean) |
| Kessler, J Craniomaxillofac Surg, 2012 (17) | NA | Oral | NA | 6 (7.5%) | Not mentioned but over 10% |
| Kessler, J Craniomaxillofac Surg, 2012 (17) | NA | All H&N | NA | NA | Authors mention no difference between centres or specialties |
| Salama, Int J Oral Maxillofac Surg, 2009 (19) | 2 (3.5%) | Oral | NA | Unclear but more than 6 (8%) | Unclear but over 21 (25%) |
| Eckardt, J Craniomaxillofac Surg, 2003 (20) | NA | All H&N | NA | Unclear but over 8% | Unclear but over 10% |
| Pohlenz, Int J Oral Maxillofac Surg, 2012 (21) | 8 (0.8%) | All H&N | NA | Unclear but over 150 (8%) | Unclear but over 200 (20%) |
| Lou, Int J Oral Maxillofac Surg, 2019 (22) | 1 (0.1%) | Oral | NA | Unclear but over 54 (7%) | 112 (11%) |
| Wang, Br J Oral Maxillofac Surg, 2018 (23) | NA but possibly 0 | Oral | NA | 8 (3.5%) | 20 (9%) |
| Sugiyama, Head Neck, 2016 (24) | NA | Oral | NA | Unclear but over 3% | Unclear but over 3% |
| Nouraei, J Plast Reconstr Aesthet Surg, 2015 (25) | 399 (3.4%) | All H&N, oral 63% | NA | Unclear but over 15% | Unclear but over 20% |
| Ho, Br J Oral Maxillofac Surg, 2012 (26) | NA | Oral | NA | Unclear but over 5% | Unclear but over 5% |
| Sweeny, Laryngoscope, 2020 (27) | NA | All H&N | NA | Unclear but over 5% | Unclear but over 5% |
| Wecks, Oral Surg Oral Med Oral Pathol Oral Radiol, 2017 (28) | NA | All H&N | NA | Unclear but over 5% | Unclear but over 5% |
| Klosterman, Otolaryngol Head neck Surg, 2015 (29) | 1 (0.5%) | Oral | NA | >10% | 20% |
| Liang, Br J Otorhinolaryngol, 2018 (30) | NA | All H&N | NA | >10% | >20% |
| Zhang, Int J Oral Maxillofac Surg, 2015 (31) | NA | All H&N | NA | Unclear but over 5% | Unclear but over 5% |
| Farquhar, Otolaryngol Head Neck Surg, 2018 (32) | NA | All H&N | NA | >10% | 44% |
| Brady, Am J Otolaryngol, 2017 (33) | 11 (1.9%) | All H&N | 5% | 15% | 45% |
| Thomas, JAMA Facial Plast Surg, 2018 (34) | Unclear | All H&N | Unclear | 225 (20%) | 54% |
| Kucur, Eur Arch Otorhinolaryngol, 2016 (35) | NA | All H&N | NA | 44 (17%) | 78 (32%) |
| Husso, J Reconstr Microsurg, 2016 (36) | NA | All H&N | NA | NA | 25% |
| Smith, Br J Oral Maxillofac Surg, 2005 (37) | 4 (1.8%) | Oral | NA | 44 (18%) | >20% |
| Dassonvile, Eur Arch Otorhinolaryngol, 2008 (38) | NA | All H&N | NA | >5% | >5% |
| Ross, J Reconstr Microsurg, 2008 (39) | NA | All H&N | NA | >5% | >5% |
H&N, head and neck; NA, not applicable.
There was great variability on the available results for the secondary outcomes. Mortality data were available in 9 studies (33%) with a perioperative mortality rate ranging from 0–3.4%. Only two studies reported readmission rates (5% vs. 7%). Unfortunately, data on return to theatre for re-exploration and Clavien-Dindho surgical complications weren’t available in the majority of the studies. Information on preop RTX was available in 9 studies (14-16,18,19,22-24,32); in one of them (15) the flap success rate was 90% with 26% of the study population being post RTX patients.
Quality of evidence
Figure 2 shows the GRADE summary of findings to assess for bias risk. As expected, the overall study quality was low or very low. Bias was serious in many outcomes due to lack of direct comparisons. There was also heterogenicity in the results from earlier literature with higher rates of complications (I2 P<0.05). Selective reporting bias (40) is assumed, as units with failure rates higher than the perceived maximum (i.e., 10%) do not publish their outcomes. The author is aware that these units exist (at least in the UK) via RCS external reviews (data not shown).
Discussion
The current systematic review, first of its kind in the medical literature, revealed a somehow unexpected finding: That surgical throughput and number of free flap cases/year is not clearly and directly related to the free flap success rate, based on the data available on the published eligible papers. This of course comes as a surprise, as one of the main arguments supporting the centralization of H&N services is the need to improve all of patients’ outcomes, including flap success rate. In other specialties, the association between volume and outcomes is very clear and has already led to reconfiguration of services (i.e., vascular surgery) (6).
Without dismissing the possibility of strong selective reporting bias (40), it seems as if the medical evidence doesn’t support the argument of a link between surgical throughput and free flap success outcomes. Furthermore, there was scarcity of available data to draw a clear correlation between volume and the secondary outcomes. Admittedly, the search algorithm used on this occasion was targeted to flap survival outcomes, and some studies looking specifically at the secondary outcomes might have been missed. I am aware of studies specifically looking at these secondary outcomes from large units in UK and Europe (41,42); these studies report complications towards the upper end of what is recorded in this systematic review. Although speculative, it seems like larger units might report higher complication rates. This of course could be linked to a stronger data collection mechanism and a more robust clinical governance, and M&M processes.
The main limitation of the current systematic review and the available data is that they are not fully representative of all the units performing microvascular free flaps for H&N reconstruction worldwide. Registration mechanisms do not exist in many countries and in those that have one, recording of data and outcomes is not always mandatory. Therefore, the threat of selective reporting bias is real. However, one cannot dismiss what is clearly shown in the literature, which is comparable outcomes between low and high-volume units.
There are a number of ways to interpret these results. From my point of view, I see them as equipoise-generating highlighting the importance of outcome reporting. We live in the era of data clarity, and this was emphasized recently with the covid19 pandemic (43). This unfortunate situation showed us how easy and quick can be to collect reliable and robust worldwide data, if there is universal will (44). I do not see why we cannot do the same for free flap H&N reconstruction. A worldwide database is feasible and welcomed; internet and digital technology can make this happen in virtually no time. The UKNFR (9) is a prime example of what a free flap registry should look like; a worldwide database like that will resolve the ambiguity around outcomes in less than a year.
This systematic review could not address the main argument favoring centralization of H&N services and H&N free flap reconstruction. This is cost and health economics. Without a doubt, collecting manpower and recourses in large centers creates several opportunities for money saving exercises (oncall rotas, fewer MDT clinics, less junior residences in one site, etc.). However, this should be weighted against potential disruption for patients, as some will need to travel further to be treated in a specialist centralized unit. Often this is accompanied by promises of better care and better outcomes. Whilst this is not entirely degraded, the results of the current systematic review call for caution when discussing about flap success outcomes. According to the literature, small isolated units have the potential to offer equally good flap success outcomes to the local population. Whether this is financially sustainable or desirable is a different story, that falls outside the scope of this manuscript.
There are a number of reasons to look at large units with high throughput in a positive way. Teaching and training are one of the main ones. Rotating in such a unit gives trainees/residences an opportunity for a swift exposure in a variety of reconstructive options in a short period of time. It also allows involvement with cases with rarer pathologies and rarer anatomical variations (the more you do the more you see). It builds up a culture of teamwork and multidisciplinary approach. There might be better access to new technology and innovation (i.e., robotic surgery, 3D printing, financially sustainable only when shared between specialties and used very frequently in a tertiary hospital). There is possibly better support from other allied health specialties (ICU, anesthetics, interventional radiology) and clinical interdependencies are clearly defined and available. A large centralized unit has kudos and higher public profile which has a positive impact on recruitment, aka service resilience. A large center can easily recruit to clinical trials, thus supporting research.
My study has several limitations. Firstly, the systematic review was contacted by a single author. However, I have significant experience in contacting systematic reviews and meta-analyses (45-47) and have published widely on the methodology of these kind of studies (40,45). Therefore, the results of the current study are reliable, despite contradicting my expectations (and my personal beliefs/wishes). However, there is still a risk of selection bias and this should be taken into account when interpreting the results. Secondly, selective reporting might have influenced the results of my review; but this could have been done in either direction (i.e., favoring large or small units) as it is currently impossible to identify and control the denominator (total number of units and number of cases/year in each of them). Thirdly, factors influencing free flap success rate are multiple, and the one chosen to record for this review (preop RTX) was found to be significantly under-reported; this might have influenced the outcomes. Lastly, it is very possible that the vast majority of units and surgeons are happy with the (arbitrary) universally accepted 95% (+/−) free flap success rate and they won’t report their results unless extremely good (i.e., approaching 100%) or forced to do so by their institution if extremely poor.
Conclusions
In conclusion, this systematic review revealed that the reported free flap success rate for H&N reconstruction is similar between units with large or small case volume. The quality of the identified studies was questionable, and the risk of selective reporting bias is lurking. This systematic review calls for caution when outcomes are used as a justification for centralizing H&N services, as literature does not seem to support this as strongly is in other surgical disciplines.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Michael Ho) for the series “Head and Neck Reconstruction” published in Frontiers of Oral and Maxillofacial Medicine. The article has undergone external peer review.
Reporting Checklist: The author has completed the PRISMA reporting checklist. Available at https://fomm.amegroups.com/article/view/10.21037/fomm-20-60/rc
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-20-60/coif). The series “Head and Neck Reconstruction” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Koumoullis H, Burley O, Kyzas P. Patient-specific soft tissue reconstruction: an IDEAL stage I report of hemiglossectomy reconstruction and introduction of the PANSOFOS flap. Br J Oral Maxillofac Surg 2020;58:681-6. [Crossref] [PubMed]
- Kyzas P. Patient-Specific Three-Dimensional Planning for Head and Neck Reconstruction: Paradigm Shift and Refuted Myths. Plast Reconstr Surg 2022;149:359e-61e. [Crossref] [PubMed]
- Melnychuk M, Vindrola-Padros C, Aitchison M, et al. Centralising specialist cancer surgery services in England: survey of factors that matter to patients and carers and health professionals. BMC Cancer 2018;18:226. [Crossref] [PubMed]
- Kovatch KJ, Hanks JE, Stevens JR, et al. Current practices in microvascular reconstruction in otolaryngology-head and neck surgery. Laryngoscope 2019;129:138-45. [Crossref] [PubMed]
- Helenius K, Gissler M, Lehtonen L. Trends in centralization of very preterm deliveries and neo-natal survival in Finland in 1987-2017. Transl Pediatr 2019;8:227-32. [Crossref] [PubMed]
- Wanhainen A, Haulon S, Kolh P. Centralization of Abdominal Aortic Aneurysm Repair - We Can No Longer Ignore the Benefits! Eur J Vasc Endovasc Surg 2020;60:500-1. [Crossref] [PubMed]
- Eskander A, Merdad M, Irish JC, et al. Volume-outcome associations in head and neck cancer treatment: a systematic review and meta-analysis. Head Neck 2014;36:1820-34. [Crossref] [PubMed]
- Khajuria A, Prokopenko M, Greenfield M, et al. A Meta-analysis of Clinical, Pa-tient-Reported Outcomes and Cost of DIEP versus Implant-based Breast Reconstruction. Plast Reconstr Surg Glob Open 2019;7:e2486. [Crossref] [PubMed]
- Hazari A, Walton P. The UK National Flap Registry (UKNFR): A National Database for all pedicled and free flaps in the UK. J Plast Reconstr Aesthet Surg 2015;68:1633-6. [Crossref] [PubMed]
- Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [Crossref] [PubMed]
- Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. Chichester (UK): John Wiley & Sons, 2019.
- Ragbir M, Brown JS, Mehanna H. Reconstructive considerations in head and neck surgical oncology: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 2016;130:S191-7. [Crossref] [PubMed]
- Gjerdevik M, Heuch I. Improving the error rates of the Begg and Mazumdar test for publication bias in fixed effects meta-analysis. BMC Med Res Methodol 2014;14:109. [Crossref] [PubMed]
- Al-Dam A, Zrnc TA, Hanken H, et al. Outcome of microvascular free flaps in a high-volume training centre. J Craniomaxillofac Surg 2014;42:1178-83. [Crossref] [PubMed]
- Spoerl S, Schoedel S, Spanier G, et al. A decade of reconstructive surgery: outcome and perspectives of free tissue transfer in the head and neck. Experience of a single center institution. Oral Maxillofac Surg 2020;24:173-9. [Crossref] [PubMed]
- Marttila E, Thorén H, Törnwall J, et al. Complications and loss of free flaps after reconstructions for oral cancer. Br J Oral Maxillofac Surg 2018;56:835-40. [Crossref] [PubMed]
- Kessler P, Poort L, Böckmann R, et al. Definition of quality indicators in microsurgery in head and neck reconstruction based on a 5-year follow-up without a loss. J Craniomaxillofac Surg 2013;41:2-6. [Crossref] [PubMed]
- Rendenbach C, Hölterhoff N, Hischke S, et al. Free flap surgery in Europe: an interdisciplinary survey. Int J Oral Maxillofac Surg 2018;47:676-82. [Crossref] [PubMed]
- Salama AR, McClure SA, Ord RA, et al. Free-flap failures and complications in an American oral and maxillofacial surgery unit. Int J Oral Maxillofac Surg 2009;38:1048-51. [Crossref] [PubMed]
- Eckardt A, Fokas K. Microsurgical reconstruction in the head and neck region: an 18-year experience with 500 consecutive cases. J Craniomaxillofac Surg 2003;31:197-201. [Crossref] [PubMed]
- Pohlenz P, Klatt J, Schön G, et al. Microvascular free flaps in head and neck surgery: complications and outcome of 1000 flaps. Int J Oral Maxillofac Surg 2012;41:739-43. [Crossref] [PubMed]
- Lou C, Yang X, Hu L, et al. Oromandibular reconstruction using microvascularized bone flap: report of 1038 cases from a single institution. Int J Oral Maxillofac Surg 2019;48:1001-8. [Crossref] [PubMed]
- Wang C, Fu G, Liu F, et al. Perioperative risk factors that predict complications of radial fore-arm free flaps in oral and maxillofacial reconstruction. Br J Oral Maxillofac Surg 2018;56:514-9. [Crossref] [PubMed]
- Sugiyama N, Takao S, Suzuki E, et al. Risk factors of thrombosis in a single method of microsurgical head and neck reconstruction: A multi-institutional study of 773 reconstructions with a free jejunal graft after total pharyngolaryngoesophagectomy for hypopharyngeal cancer. Head Neck 2016;38:1688-94. [Crossref] [PubMed]
- Nouraei SA, Middleton SE, Hudovsky A, et al. Role of reconstructive surgery in the management of head and neck cancer: a national outcomes analysis of 11,841 reconstructions. J Plast Reconstr Aesthet Surg 2015;68:469-78. [Crossref] [PubMed]
- Ho MW, Brown JS, Magennis P, et al. Salvage outcomes of free tissue transfer in Liverpool: trends over 18 years (1992-2009). Br J Oral Maxillofac Surg 2012;50:13-8. [Crossref] [PubMed]
- Sweeny L, Topf M, Wax MK, et al. Shift in the timing of microvascular free tissue transfer failures in head and neck reconstruction. Laryngoscope 2020;130:347-53. [Crossref] [PubMed]
- Weckx A, Loomans N, Lenssen O. Perforator free flaps in head and neck reconstruction: a single-center low-volume experience. Oral Surg Oral Med Oral Pathol Oral Radiol 2017;123:429-35. [Crossref] [PubMed]
- Klosterman T, Siu E, Tatum S. Free flap reconstruction experience and outcomes at a low-volume institution over 20 years. Otolaryngol Head Neck Surg 2015;152:832-7. [Crossref] [PubMed]
- Liang J, Yu T, Wang X, et al. Free tissue flaps in head and neck reconstruction: clinical application and analysis of 93 patients of a single institution. Braz J Otorhinolaryngol 2018;84:416-25. [Crossref] [PubMed]
- Zhang C, Sun J, Zhu H, et al. Microsurgical free flap reconstructions of the head and neck region: Shanghai experience of 34 years and 4640 flaps. Int J Oral Maxillofac Surg 2015;44:675-84. [Crossref] [PubMed]
- Farquhar DR, Masood MM, Pappa AK, et al. Predictors of Adverse Outcomes in Free Flap Reconstruction: A Single-Institution Experience. Otolaryngol Head Neck Surg 2018;159:973-80. [Crossref] [PubMed]
- Brady JS, Crippen MM, Filimonov A, et al. The effect of training level on complications after free flap surgery of the head and neck. Am J Otolaryngol 2017;38:560-4. [Crossref] [PubMed]
- Thomas WW, Brant J, Chen J, et al. Clinical Factors Associated With Reoperation and Prolonged Length of Stay in Free Tissue Transfer to Oncologic Head and Neck Defects. JAMA Facial Plast Surg 2018;20:154-9. [Crossref] [PubMed]
- Kucur C, Durmus K, Uysal IO, et al. Management of complications and compromised free flaps following major head and neck surgery. Eur Arch Otorhinolaryngol 2016;273:209-13. [Crossref] [PubMed]
- Husso A, Mäkitie AA, Vuola J, et al. Evolution of Head and Neck Microvascular Reconstructive Strategy at an Academic Centre: An 18-Year Review. J Reconstr Microsurg 2016;32:294-300. [Crossref] [PubMed]
- Smith GI, O'Brien CJ, Choy ET, et al. Clinical outcome and technical aspects of 263 radial forearm free flaps used in reconstruction of the oral cavity. Br J Oral Maxillofac Surg 2005;43:199-204. [Crossref] [PubMed]
- Dassonville O, Poissonnet G, Chamorey E, et al. Head and neck reconstruction with free flaps: a report on 213 cases. Eur Arch Otorhinolaryngol 2008;265:85-95. [Crossref] [PubMed]
- Ross GL, Ang S W EE, Lannon D, et al. A ten-year experience of multiple flaps in head and neck surgery: how successful are they? J Reconstr Microsurg 2008;24:183-7. [Crossref] [PubMed]
- Kyzas PA, Loizou KT, Ioannidis JP. Selective reporting biases in cancer prognostic factor studies. J Natl Cancer Inst 2005;97:1043-55. [Crossref] [PubMed]
- McMahon JD, MacIver C, Smith M, et al. Postoperative complications after major head and neck surgery with free flap repair--prevalence, patterns, and determinants: a prospective cohort study. Br J Oral Maxillofac Surg 2013;51:689-95. [Crossref] [PubMed]
- Perisanidis C, Herberger B, Papadogeorgakis N, et al. Complications after free flap surgery: do we need a standardized classification of surgical complications? Br J Oral Maxillofac Surg 2012;50:113-8. [Crossref] [PubMed]
- Ioannidis JPA. Coronavirus disease 2019: The harms of exaggerated information and non-evidence-based measures. Eur J Clin Invest 2020;50:e13222. [Crossref] [PubMed]
- Bejjani A, Burt L, Washington C, et al. Using a Collaborative, Virtual Discussion Platform to Mobilize Oncologic Expertise for the COVID-19 Pandemic. JCO Clin Cancer Inform 2020;4:794-8. [Crossref] [PubMed]
- Kyzas PA, Denaxa-Kyza D, Ioannidis JP. Almost all articles on cancer prognostic markers report statistically significant results. Eur J Cancer 2007;43:2559-79. [Crossref] [PubMed]
- Riley RD, Hayden JA, Steyerberg EW, et al. Prognosis Research Strategy (PROGRESS) 2: prognostic factor research. PLoS Med 2013;10:e1001380. [Crossref] [PubMed]
- Kyzas PA. Use of antibiotics in the treatment of mandible fractures: a systematic review. J Oral Maxillofac Surg 2011;69:1129-45. [Crossref] [PubMed]
Cite this article as: Kyzas P. The impact of volume and surgical throughput on outcomes in head and neck reconstruction: a systematic review. Front Oral Maxillofac Med 2022;4:23.


