
Indications for alloplastic total joint replacement in obstructive sleep apnea patients requiring maxillomandibular advancement
Introduction
The most common of the sleeping disorders in the United States is obstructive sleep apnea (OSA). Occurring in approximately 30% of males and 15% of females (1-4). OSA is associated with increased cardiovascular and respiratory disease, increased morbidity, and substantially increased medical costs (5). Those suffering from OSA often experience a collapse in their airway, which in turn provokes the body to push the lower jaw forward to open up the airway (6). This constant motion by the temporomandibular joint (TMJ) throughout the night can cause stress and tension on the joints and increase the likelihood of sleep apnea or exacerbate it (7). Degenerative joint diseases, trauma and any pathology that leads to condylar resorption all have a similar end result in a retrusive mandible (8,9).
As temporomandibular diseases, that specifically affect the condyle, progress and cause more damage via resorption and remodeling to the joints the altered topography of the joints in turn leads to a loss in both an anterior-posterior and vertical height projection of the mandible. The loss of said projections then culminates into a collapse of the posterior oropharyngeal airway, which also worsens or leads into a development of OSA (10-13). It has also been shown in other studies that the prevalence of temporomandibular joint disorders (TMDs) in patients with already established OSA is significantly higher than in patients with untreated OSA (14). In cases of OSA unrelated to TMJ damage, traditional maxillomandibular advancement (MMA) has shown high success rates to improve the volume of the airway (15). However, in patients with TMJ damage or involvement, the movements may not be possible or stable due to the degenerative effects on the condyles of the mandible. In these cases, MMA can be achieved with total joint prostheses (TJPs) to replace the damaged joint(s). The advantage of this method is that a surgeon can improve the posterior airway volume, reducing the collapse, thus treating the OSA, and preventing any potential relapse (16-18).
This review will discuss the perioperative diagnosis, workup, and treatment for patients with OSA as a result of TMJ pathology. The main surgical technique will involve TMJ total joint replacement (TJR) surgery.
Specific indications
Indications for the use of prosthetic joints to treat OSA include conditions that cause degeneration or resorption of the condyles. These include juvenile idiopathic arthritis, idiopathic condylar resorption, trauma that results in bony ankylosis of the joint, and degenerative joint diseases (19). Another type of case that results in constricted airway and eventual OSA are post operative orthognathic surgery cases that have relapsed (20). This stresses the importance of performing a thorough TMJ exam.
Skeletal relapse can also lead to malocclusions and is a concern due to the large amount of advancement that places tension on oral and pharyngeal tissues and ultimately a degenerated joint. These same forces attempt to pull the mandible back to its original position, however it does not do so in a linear vector and thus the posterior forces also cause a downward pull as well, all of these forces acting in concert result in anterior apertognathia.
The relationship between OSA and TMJ disease
There have been several studies that demonstrate a relationship between patients that suffer from OSA, and also have concomitant TMJ disease. In these studies multiple types of groups of patients were studied. Some of the results showed that in patients with chronic OSA with two or more symptoms (e.g., daytime sleepiness, snoring) there was an increased 73% chance of the same patients also having TMJ disease. Similarly, this same study also conducted a case control design, which demonstrated that those patients with chronic TMJ diseases were three times more likely to have signs of OSA (low to severe). Another study, involving 87 adults who were diagnosed via polysomnography (PSG), as having mild or moderate OSA. It was found that 32 (36.8%) had some type of TMJ disease, based on the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD). Yet another study, involving 11 of 53 adults (28%) that also demonstrated patients with myofascial pain syndrome (according to RDC/TMD) were also diagnosed by PSG as having OSA as well (21). Granted, correlation does not equal causation, the prospective cohort findings imply that OSA contributes to the onset of painful TMJ disease symptoms.
With regards to treatment of OSA with concomitant TMJ disease, reports of mandibular advancement with simultaneous bilateral TMJ replacement have been reported successfully (22). In this case, computed tomography (CT) showed that the condylar hypoplasia, resultant micrognathia, and decreased retrolingual and retropharyngeal airway space were all significantly improved with the surgical procedures. However, these results were based on clinical assessment and the Epworth Sleepiness Scale, and without the use of PSG. There was a study that did involve PSG in evaluating the relationship between TMDs (TMJ disease and myofascial pain) and OSA. In this particular study of a group of women (170; of which 146 had clinically diagnosed TMD and the remaining serving as the control group), the TMD cases elucidated a relationship between pain ratings and sleep parameters. They determined that myofascial pain and other TMJ diseases were strongly associated with increased sleep fragmentation and increased respiratory effort related arousals (RERAs) (23). In yet another study conducted in Singapore, a group of patients where clinically diagnosed with TMJ disease and compared to those with OSA/upper airway resistance syndrome (UARS). A significantly high correlation was found to the effect that the authors recommended screening for OSA/UARS in patients with chronic TMJ diseases (24).
A brief history of MMA
Orthognathic surgery was first described as a technique to treat sleep apnea as early as 1979. The authors of this study used mandibular advancement alone. The study described three cases of mandibular advancement as successful treatment modality of “hypersomnia sleep apnea” (25). In later studies, the maxilla would be added in the advancement process in order to maintain occlusion (26).
MMA has been shown to be an effective treatment for OSA with a success rate of up to 86%. Many patients with high residual Apnea-Hypopnea Index (AHI) or Respiratory Disturbance Index (RDI) after other unsuccessful surgical procedures for OSA are likely to benefit from MMA. AHI is a scale that that tells whether you have a sleep disorder such as apnea and, if so, how serious it is. A sleep apnea is when you stop breathing for 10 seconds or more while you’re asleep. A similar disorder, hypopnea, is a partial loss of breath for 10 seconds or longer. The RDI is a similar measure to AHI, but it also includes the number of respiratory effort-related arousals per hour of sleep (in addition to apnea and hypopnea events) (27). There are other non-surgical treatments for sleep apnea surgery that should be attempted first, such as continuous positive airway pressure (CPAP) and mandibular advancement splints (MAS). There are studies that do show that surgery is a superior modality, especially if CPAP and MAS are inadequate (28).
In cases of TMJ disease with concomitant OSA, the bilateral sagittal split osteotomy (BSSO) is insufficient at targeting the underlying cause of soft tissue collapse and retrognathia. Since the case here is alteration of the morphology of the condyle and/or disc, the BSSO obviously does nothing to address this. If the TMJ severely degenerated, then alloplastic prosthesis replacement is in order to correct the upper airway collapse, any deformities present, and correct any malocclusions. It has been shown that total joint prosthesis has had increasing success rates in terms of stability (29,30).
In addition, due to the new and improved designs and components, there has also been reports of improvements in treating dentofacial deformities and TMJ pathology. Given this information, alloplastic TJR with total joint prosthesis as evolved into aiding concomitant orthognathic surgery in order to treat the underlying causes of collapsed airway and OSA.
Preoperative evaluation
The planning and objectives of MMA with TJPs is very similar to traditional orthognathic planning which includes detailed patient history, physical exam, radiographic analysis, clinic photographs, and model analysis (it is recommended to utilize a preliminary virtual surgical planning (VSP) at this stage if able to). The clinical exam includes both a section for assessing OSA and assessing TMJs. When examining the OSA component, the patient will require a thorough exam of the nasal passages, taking note of the septum and any deviations, observing the turbinates in case they are enlarged. Looking at the oropharyngeal spaces, and the retroglossal region taking note of the uvula, tonsils (if present), tongue size and position, as well as the occlusal classification. For the TMJ exam; this includes palpation of the muscles of mastication, palpation of the condyles, auscultating for audible clicking, crepitus, maximal incisal opening, deviation or deflection upon opening, and a Mahan test. The exam for the patients mentioned in this review were all performed by the same surgeon (RM). In addition to the expected diagnostic tools, magnetic resonance images (MRIs) more specifically give information of the soft tissues and disc of the TMJ complex, and a drug induced sleep endoscopy (DISE) can inform the surgeon more about the nature of the obstruction itself. The information from a DISE can often tell the surgeon which treatment modality would best serve the patient (i.e., MMA vs. MMA with uvulopalatopharyngoplasty) (31).
Classically speaking, the minimum amount of advancement for both the upper jaw and lower jaw to achieve predictable results in patients with OSA is 10 mm. This can lead to a decrease in AHI (32-35). However, with counterclockwise rotation, this is usually exceeded in order to achieve adequate and stable postoperative results at pogonion. In other words, custom patient fitted TMJ prosthesis allows for even greater advancements than other mandibular osteotomies and thus a greater increase in airway volume (36-39). An important distinction between the treatments for OSA, MMA or total joint prosthesis with a maxillary osteotomy, is that patients in the total joints category are having their mandible advanced because of a destructive or degenerative process (40-43). Patients with oropharyngeal collapse caused by TMJ degeneration require both substitution of the horizontal projection of the mandible as well as substitution of the vertical part of the ramus and reclamation of the occlusal plane (approximately 8°).
Patients that have developmental deformities due to TMJ pathologies have discerning patterns of facial development. As the condyles resorb, this pulls the mandible posteriorly developing retrognathism and a high mandibular plane angle, the maxilla will adapt and compensate to match the mandible. A treatment that will correct such a case would involve the mandible moving in a counterclockwise fashion, the maxilla would have to be surgically down grafted and rotated in the similar manner. In patients with later staged TMJ degenerative diseases, the maxilla may be in an orthognathic position whereas the mandible is retrusive, therefore in these cases the maxilla does not need a Le Fort osteotomy. Nonetheless, a DISE would be necessary to rule out obstruction of the airway at the level of the soft palate which may necessitate other soft tissue surgical procedures.
In evaluating the maxilla, one should determine if the maxilla is constricted in the transverse dimension. If this is the case and the maxilla is not operated on, the tongue will not have enough space to fit passively on the roof of the mouth and fall posteriorly during sleep. A useful tool to aid in determining the amount of expansion needed would be a preliminary VSP. In doing so, this allows the surgeon to decide if there should be a two staged surgery with a surgically assisted rapid palatal expansion (SARPE) followed by a Le Fort, or a segmental Le Fort. In general, a segmental Le Fort can be done safely to expand the maxilla up to 10–12 mm.
History and physical
The history and exam for these types of patients consist of ascertaining TMJ symptoms, when they began, are they worsening. Some specific questions to ask of patients that will provide useful information include: has the patient had previous orthognathic surgery? Has the patient had previous orthodontic therapy? Does the patient have parafunctional habits? Is there a family history of immunological or connective tissue disease?
The exam includes an evaluation of facial asymmetry. When viewing the patient from a profile view, the patient’s head should be oriented such that the Frankfort Horizontal plane is parallel to the floor. The purpose for this is to have a reproducible head position which is of the utmost importance in order to calibrate outcomes. The clinician should assess for dental and skeletal class I, II, or III. Observe any transverse cants or cross bites. Take note of the occlusal plane angle. Are there any premature contacts in the posterior region (patients with condylar resorption often have decrease in vertical ramus height)? Assess for TMJ issues by palpation for potential crepitus, note the absence or presence of clicking or popping. Assess for any myofascial components by completing a musculoskeletal exam of the masseters, medial pterygoids, and temporalis muscles. Followed by documentation of maximum incisal opening (MIO) and lateral excursive movements.
Imaging
Most surgeons begin with a panoramic. This can provide some initial screening information, such as the presence of arthritis but cannot elucidate the extent of disease. A CT or a cone beam computed tomography (CBCT) imaging provides superior 3D analysis of the bony structures. The patient will need either of these in order to obtain a patient fitted custom TMJ prosthesis (the scan should be planned with less than 1 mm cuts).
Just as traditional orthognathic surgery necessitates cephalometric analysis, as does combined MMA + TJR. Some common features to notice in patients with TMJ disease include; retruded mandible, high angle plane of occlusion, hypoplasia of the posterior maxilla, skeletal class II, dental class II malocclusion, and anterior apertognathia. In addition to these imaging modalities, the soft tissues and articular disc will need to be evaluated as well. This is where MRI studies are of significance from a preoperative evaluation. Some authors suggest obtaining MRIs when the CTs or screening radiographs do not show advanced bony changes (44). This makes logical sense as sometimes there are cases wherein displacement of the disc, especially without reduction, exacerbates a condylar resorption and the displacement can be noticed before the bony changes. MRI assessment should be an integral part of the presurgical evaluation for any case being planned for significant advancement.
Types of prosthesis systems
There are two types of prosthesis systems currently available in the US. They are stock (Zimmer Biomet, Jacksonville, FL, USA) and patient fitted custom prosthesis (TMJ Concepts, Ventura, CA, USA). The main disadvantages of the stock prosthetics include the need for bone contouring to allow the intaglio surface of the fossa component of the prosthetic to fit, which can add time to the surgery (45). There is also the issue with the large degree of anterior advancement with counterclockwise rotation. The current lengths of the stock prosthesis come in 45, 50, 55 mm (46). The amount of advancement, and counter-clockwise (CCW) rotation needed to correct the constricted airway, especially due to condylar resorption, to reposition the mandible often exceeds 55 mm. Another caveat of the stock prosthesis is that it does not have a posterior stop in the fossa compartment, therefore it is prone to posterior dislocation of the condylar component of the prosthesis (47). The relative advantage of the stock prosthesis is the less cost compared to the patient fitted.
In comparison, the custom patient fitted prosthesis fits intimately with the patient’s anatomy, thereby obfuscating the need to contour the patient’s fossa component. This also increases the chances for successful osseointegration of the implant. Since there is no need for altering the anatomy, this also decreases surgery time. The custom design also allows the accommodation of the large counterclockwise and anterior movements. More importantly, there are both a posterior and anterior stop, lessening the possibility of dislocation.
Surgical planning with computer aided surgical simulation (CASS)
Traditional model surgery is becoming more a relic of the past given the advent of VSP. As part of the workup for the TMJ + MMA surgery, one will need to obtain either a CBCT or a medical grade CT (<1 mm cuts). A stereolithic 203 model will be made based on the images, and provided to the surgeon for the prosthesis component. The prosthesis company will also upload the imaging data to create a 3D model. Most companies use Digital Imaging and Communications in Medicine or DICOM. DICOM is essentially an international standard to communicate and manage medical images and data. Also, either dental casts or intraoral scans can be sent to the TMJ company, which record the occlusion, to aid in fabrication. Splints will also be made from this data.
A lateral cephalogram analysis is traced and recorded. Most imaging software is capable of aiding the surgeon in this task. The software allows the surgeon to correct the deformities by mimicking the effects of MMA. The joint prosthesis company will then fabricate a stereolithic model. This model will show the maxilla and mandible in their final positions. From here, the model is sent to the surgeon for any modifications deemed necessary. At this stage, the surgeon must make sure enough space is adequate between the ramus and fossa to accommodate the prosthesis, usually 18–20 mm. The models are then sent back to the TMJ prosthesis company, who will send images of modifications made, the surgeon then approves before the final prosthesis is then fabricated. It will later be sent to the hospital along with an associated surgical kit (48).
Surgical techniques
Anesthetic considerations
Patients with OSA often have multiple comorbidities that can lead to the difficulty of inducing and maintaining anesthesia. These comorbidities can include: obesity, coronary artery disease, hypertension, pulmonary hypertension, diabetes, and a decreased functional residual capacity from a pulmonary standpoint. This can lead to a precipitous desaturation. In patients with diabetes it is recommended that their preoperative HbA1c levels are at or below 7%. It has been demonstrated in orthopedic literature that patients undergoing TJRs for knees and hips, are at increased risk for periprosthetic joint infections (49). For these reasons it is recommended that surgery for OSA patients be done in a surgical setting that has the appropriately trained staff to handle such medically complex patients. For patients receiving MMA plus TMJ TJR, it is recommended that they receive at least one overnight stay for observation.
For these patients nasotracheal intubation is the usual preferred method. For select patients, with inability to open due to ankylosis, this procedure is performed with the aid of fiber optics, and at times awake. It should also be mentioned that a longer nasotracheal tube should be used as during the mobilization of the maxilla, the tube may become displaced.
Hypotensive anesthesia should be utilized during the Le Fort osteotomy section of surgery. Any blood chemistry imbalances, such as metabolic acidosis, must be corrected during surgery and monitored afterwards.
Some have advocated for the use of perioperative CPAP. There are no specific studies that show any benefit or harm with regards to the use of CPAP preoperatively and their effects on orthognathic or TMJ + orthognathic surgery. It is recommended to not use CPAP for at least two weeks postoperatively in order to avoid subcutaneous emphysema.
Single stage or two stage surgery
When determining whether to do the ablative portion of the surgery followed by the total joint prosthesis in a single visit one should consider the following: what is the nature of the pathology of the TMJ itself? In other words, whatever the underlying etiology causing the deformity of the joint(s), will help dictate whether the surgeries should be done in one or two stages. For example, if the patient has septic arthritis, or a foreign body giant cell reaction, it would be prudent to perform the resection of the condyles immediately, place a temporary acrylic spacer, and plan for TMJ reconstruction at a later time. This would be the case so as to prevent any possible systemic infection or sepsis from occurring. Patients with tumors present in the condyle would also benefit from arthroplasty of the joint followed by later reconstruction with the prosthesis as there is concern for possible tumor seeding. Delayed reconstruction after resolution of an infection, or tumor resection, is usually utilized with a two-stage approach to account for the uncertainty of resection margins. As the presence of infection would compromise any immediate graft. There has been some research on the use of custom antibiotic impregnated spacers that show promise (50). In general, it is recommended that performing single stage surgery, especially in cases involving simultaneous maxillary osteotomies, and only doing two stage surgery when pathology of the joints dictates otherwise.
Mandible first or maxilla first surgery
In performing the maxillary surgery first, the Le Fort osteotomy is done with repositioning of the maxilla, followed by rigid fixation, then the TMJ surgery is performed. If this sequence is done then there will need to be at least two sets of instruments in order to prevent contaminating the joints. If the CCW rotation is extensive the posterior maxillary segment may collapse due to the lack of posterior rigid fixation. The anterior maxillary rigid fixation is not stable enough alone to keep the maxilla in place during surgery. This would most likely occur during the repositioning of the mandible after the condylectomy has been done. In other words, the posterior maxilla will collapse prior to the TJR prosthesis placement which will result in an occlusal plane discrepancy. Whereas if the TMJ surgery is done first, this will allow for only one set of instruments to be needed and after the prosthesis is in place the maxilla can now be set to a stable mandible. The joint prostheses are superior in stability compared to the maxillary rigid fixation. Extra care must be taken when performing the TMJ surgery first to ensure that the prosthetic condyles are still appropriately seated during the maxillary osteotomies, as they can become dislocated. This can be done by placing gentle posterior and superior pressure at the angle of the mandible, just as one would do when fixating a BSSO.
Prepping for surgery
The following are outlined steps for surgical technique. The need for sterility and avoidance of contamination cannot be overstressed.
The patient will have nasotracheal intubation. It is recommended that an extended Parker nasal right angle endotracheal (RAE) tube be used as the chances for intraoperative extubation are lessened. Once intubated the tube is secured, either with silk suture through the septum or via a maxillofacial headwrap. Any hair that may be in the surgical field would be shaved at this point. Patients with long hair are recommended to braid their hair the night prior. Once the nasotracheal tube is secured, intermaxillary fixation devices are placed (such as arch bars or IMF screws), but the patient is not placed into maxillomandibular fixation at this time. It is recommended that instruments be placed on a separate “dirty”, Mayo stand kept separate from the main instrument tables. This will be re-used later during the case.
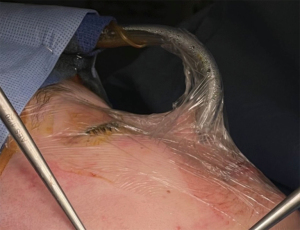
At this point the use of clear adhesive dressing (i.e., Tegaderm) is placed over the mouth, nose, and eyes to seal this area from the TMJ area. Alcohol pads can be used to prep the preauricular region, then local anesthetic with vasoconstrictor is injected at each preauricular site subcutaneously, care is taken not to inject into layers deeper than this as it could affect the facial nerve. Cotton pledgets, ear wicks, or cotton moistened with mineral oil are placed in the external auditory canal. From this point, the patient is now traditionally prepped and draped as would be similar to an orthognathic surgical case (Figure 1).
Incisions
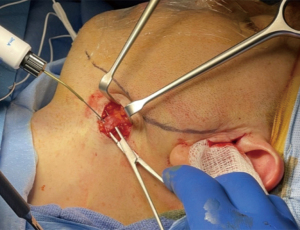
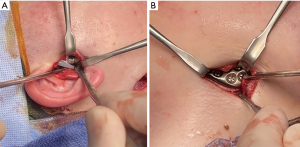
In order to achieve full visualization of the joint, disc, condyle and part of the ramus necessary in order to perform the surgery safely, there are two incisions typically taught. These are the preauricular and endaural incisions. In the authors’ experience the endaural, although more meticulous, tends to lead to less postoperative complications. This is because the superficial temporal vessels, branches of the facial nerve, and auriculotemporal nerve will be within the flap created, or anterior to it. Dissecting into a supra tragal plane is essentially an avascular plane (Figure 2). When approaching the superficial temporalis fascia, dissection can be taken down to the periosteum covering the zygomatic arch. Subperiosteal dissection in the anterior direction towards the articular eminence is a safe area and will then bring the joint capsule into view (Figure 3). In order to confirm that one is at the level of the capsule, 1 to 2 mL of local anesthetic with vasoconstrictor is injected into the superior joint space, and in doing so observe if the mandible moves forward.


Condylectomy
With the joint capsule identified, beginning at the posterior aspect of the condylar neck a vertical incision superiorly towards the condyle is made. Using curved Freer or periosteal elevator, sub periosteal dissection is taken anterior, then posterior in a circumferential manner both above and below the proposed site of condylectomy. With the Freer’s in place retracting the soft tissue, a piezoelectric hand piece is used to make a horizontal osteotomy through both cortices. The osteotomy should be low enough to remove enough of the condyle and condylar neck to accommodate the fossa component of the prosthesis. This is usually at the level of the coronoid notch. If indicated a coronoidectomy may be performed in similar fashion. The use of a piezoelectric system is recommended because it will result in less soft 339 tissue damage and better control of bleeding compared to other instruments used (51) (Figure 4). Care is taken to avoid damage to the internal maxillary artery. Once complete, a T-handle osteotome, or blunt instrument is placed into the osteotomy, turned to cause fracture. The condyle with the neck is grasped with forceps and removed. The attachment of the lateral pterygoid muscle can be dissected off with a periosteal elevator. If not removed at the same time as the condyle, then the disc is removed at this time. Further debridement of soft tissue is done at this time as well. There needs to be a minimum of 20 mm between the fossa and leftover ramus component.

Submandibular incision
The advantage of this incision is that it allows access to both the lateral and inferior portions of the ramus. This will also allow for placement of the condylar component of the TMJ prosthesis. A 1.5 to 2 cm incision is placed 2 cm inferior to the inferior border of the mandible so that the marginal mandibular branch of the facial nerve is protected. Dissection is done through the platysma with scissors, or Bovie electrocautery. Nerve monitoring is recommended (Figure 5). Continued medial dissection of the medial pterygoid is also recommended as the movements of the mandible will be large and stripping of the muscle will allow for greater mobility. Sub periosteal dissection of the masseter is done until it meets with the superior extent the first incision. Steps are repeated on the contralateral side, now with a fully mobile mandible, it is placed into an intermediate splint and placed into intermaxillary fixation. It is important to notice that with the large movements of the mandible that the inferior alveolar nerve is greatly stretched even so to the point of possible permanent paresthesia.
Now the patient is placed into maxillomandibular fixation. It is paramount that the contents of the oral cavity do not contaminate the endaural or submandibular incisions. This can be done with towels and drapes. Another set of instruments may need to be used as this part of the surgery is non sterile. The previously placed Tegaderm over the mouth is incised and entered. Intermaxillary fixation with the intermediate splint in place. Care is taken to ensure there is no movement during this process. Then the Tegaderm is replaced and patient is prepped again.
Hardware fixation
The fossa component of the prosthesis is placed first. The titanium 373 end is placed against the bone with the polyethylene (white) portion facing inferiorly. There is a fossa seating tool that is used to place and hold the fossa in position while placing in screws. The condyle should be placed in the appropriate position, this is superior and posterior against the posterior stop of the fossa component and also centered medio-laterally. Now with both components placed appropriately, rigid fixation is applied via bicortical screws. This can be aided with drill guides or trocar as seen fit. It is recommended to use slow speed drills with copious saline irrigation so as to prevent devitalization of the bone. Usually, screws with 2 mm diameters that are self tapping are recommended (Figure 6). Should it be necessary, TMJ Concepts does also provide 2.3 mm rescue screws. As many screws as feasible should be placed, but not all screws need to be fixated in order to achieve appropriate fixation. Usually 3 screws in the fossa component and 7 screws in the ramus component are adequate. Make sure all screws that are placed are tight with a hand screw driver. If this is a bilateral case the same steps are repeated on the contralateral side. Fat harvested from the abdomen is then placed circumferentially around the prosthetic condyle so as to prevent heterotopic bone formation (52-54). Copious saline and betadine irrigation is recommended at both the endaural and submandibular incisions. The incisions are closed in layered fashion.
Maxillomandibular fixation is now released. Taking note if there is any change in occlusion. The mandible is motioned to note if it fits passively into the intermediate splint. If a Le Fort I osteotomy (single piece or segmented) is planned, it would be performed next. In order to aid in postoperative comfort, the use of elastics is implemented.
Whichever means of occluding the external auditory canal(s) was placed, it is removed at this time. It is recommended to place a Barton type dressing for 8–12 hours. Placement of nasal trumpet airway in one or both nostrils may also be placed to aid in oxygenation postoperatively.
Le Fort I osteotomy
After skin closure, if maxillary osteotomies are required they are performed at this time. As the procedure is no longer sterile it is ok to use the instruments on the surgical field, and the procedure can be performed without concern for contamination. To place the maxilla in the correct position, a Kirschner or K-wire, is placed at the nasion and cut to 1 cm from the skin. Then measured at the incisal aspects of teeth #8 & #9. The Le Fort osteotomy is performed with a reciprocating saw or piezoelectric handpiece, about 4 mm apical to the suspected roots. If a segmental Le Fort I is planned the beginning of the interdental osteotomies are started at this point and completed after the maxillary down fracture. A double guarded osteotome is then used to separate the septum from the maxilla. Single guarded osteotomes are used at the lateral nasal walls. A curved osteotome is used to separate the pterygoid plates. Maxillary down fracture is completed. It should be noted that with prosthetic joints, standard methods of down fracture may be too forceful and could dislocate the condyles, therefore the down fracture should be done in a slow and careful fashion. If visualized the descending palatine arteries may be sacrificed.
Care must be taken as the TMJ prosthesis can be dislocated during the maxillary down fracture. Once mobilized the maxilla is then placed into final occlusion with the final splint. Closure of the incision proceeds using 3-0 vicryl suture for an alar cinch, followed by 3-0 chromic gut suture for a continuous V-Y closure. Kirschner wire is then removed.
Case examples
Case #1
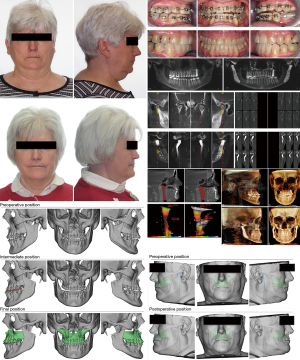
Patient is a 36-year-old male presented to our outpatient clinic with chief complaint of having sleep apnea. This was confirmed with a preoperative PSG presenting moderate sleep apnea. Patient endorsed excessive daytime somnolence, inability to perform his daily duties at work, daytime morning headaches. In addition to these OSA symptoms, the patient also complained of pain about both of his TMJs, limited opening of 14mm without pain and 34 mm with pain on opening. There was bilateral crepitus present as well. The patient also displayed class II malocclusion, an anterior open bite, and evidence of bruxism. On radiographic examination there was heterotopic bone formation and arthritic changes involving osteophytes about both condyles. The preoperative phase involved orthodontic treatment to level and alignment of the arches and creating space between the lateral incisors and canines of the maxilla bilaterally to facilitate interdental osteotomies. The surgical phase included multiple osteotomy Le Fort I, bilateral condylectomies, reconstruction of the TMJ with custom prosthesis, genioplasty with advancement, counterclockwise rotation and MMA, and an abdominal fat harvest. Patient received a post operative sleep study which showed a decrease in AHI to 0 and RDI to 2.0 (Figure 7).

Case #2
Patient is a 49-year-old female presented to our outpatient clinic with the chief complaint of having trouble in sleeping. This was confirmed with a preoperative PSG presenting severe sleep apnea. Patient endorsed excessive daytime somnolence, inability to perform her daily duties at work, and daily headaches. Additionally, the patient also had complaints of pain in her TMJs (left > right), patient limited opening of about 15 mm without pain and 37 mm with pain on opening. Bilateral crepitus was present. On radiographic examination there were arthritic changes in both condyles with osteophytes about the left condyle, flattening of the heads of both condyles, and decreased joint space bilaterally. The preoperative phase involved orthodontic treatment to level and alignment of the arches and creating space between the lateral incisors and canines of the maxilla bilaterally to facilitate interdental osteotomies. The surgical phase included multiple osteotomy Le Fort I, bilateral condylectomies, reconstruction of the TMJ with custom prosthesis, genioplasty with advancement, counterclockwise rotation and MMA, and an abdominal fat harvest. Patient received a preoperative sleep study which showed both RDI and AHI to be 33 and a postoperative AHI of 2.0 (Figure 8).
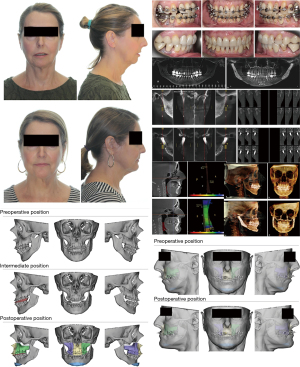
Case #3
Patient is a 65-year-old female who presented to our clinic with a chief complaint of having difficulty in sleeping; and that was confirmed with a preoperative PSG presenting severe sleep apnea. Her AHI was 42. Patient endorsed excessive daytime somnolence, periods of time that were lost to her as she felt she “dozed off”, and chronic fatigue throughout the day. Patient was intermittently compliant with a CPAP device but endorsed little improvement and difficulty in wearing the device. Additionally, the patient also had complaints of pain in her TMJs (right > left), patient limited opening of about 20 mm without pain and 29 mm with pain on opening. Bilateral crepitus was present. On radiographic examination there were arthritic changes in both condyles with osteophytes about both condyles, subchondral cysts, and flattening of the heads of both condyles. The preoperative phase involved orthodontic treatment to level and alignment of the arches. The surgical phase included Le Fort I osteotomy, bilateral condylectomies, reconstruction of the TMJ with custom prosthesis, counterclockwise rotation and MMA, and an abdominal fat harvest. Patient’s postoperative AHI was <5, her opening increased to 41 mm, her pain was resolved and she endorsed improvement of her original OSA symptoms (Figure 9).
Conclusions
MMA has been a well-established treatment modality for OSA for years now with an 86% success rate, the highest rate compared to all the other procedures performed. Patients who have MMA as a result of sleep apnea, should have their TMJs examined for possible pathology, given that the joints are paramount for stability and success of MMA. This is true in the case of traditional MMA surgery without a concomitant joint procedure, but is especially true in patients who require a prosthetic replacement. Patients who have had MMA surgery without joint replacements in the setting of joint pathology can have a higher likelihood of relapse and unsatisfactory results.
There are not many studies looking at sleep studies done post operatively specifically in patients with MMA + TJP but we know that it is skeletally stable. A particular studied conducted demonstrated the stability and anatomical changes which increased the oropharyngeal airway after MMA with TMJ prosthesis (20). Additional studies have shown in a patient with condylar atrophy due to juvenile idiopathic arthritis, there was an increase in the retrolingual airway and any stated symptoms based on the Epworth Sleepiness Scale, as well as a significant decrease in AHI. However, this was for a single patient (22). A study conducted by Mishima and colleagues looked at 6 patients who had condylar resorption secondary to rheumatoid arthritis and measured certain respiratory parameters to determine if they improved. After surgery, which only included mandibular advancement with TJR, patients reported improvement in symptoms such as stertor and daytime somnolence. There was also an improved ability to masticate solid food. Their report also demonstrated via the postoperative cephalograms that both the posterior airway space and ramus height were greatly increased and stable at the one year follow up appointments. Mean oxygen saturation also significantly improved 1 month post op. However the AHIs did not change significantly (16). This highlights the importance of considering the advancement of both jaws and utilizing counterclockwise rotation in the treatment of OSA patients requiring MMA + TJR.
Given the relative scarcity of research utilizing a combination of airway measurements, DISE, and PSG, there is still more to discover in relation to treating OSA patients with TMJ pathologies with TMJ prosthesis replacement, counterclockwise rotation of the mandible and concomitant maxillary surgery. In the evaluation of patients who need MMA for OSA, the diagnostic information from the TMJ should not be overlooked as it is the foundation for the airway, profile and occlusion.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Louis Mercuri) for the series “Indications for Alloplastic TMJ Replacement in Maxillofacial Surgery—an evidence-based review of the literature” published in Frontiers of Oral and Maxillofacial Medicine. The article has undergone external peer review.
Peer Review File: Available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-14/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-14/coif). The series “Indications for Alloplastic TMJ Replacement in Maxillofacial Surgery—an evidence-based review of the literature” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this article and accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Peppard PE, Szklo-Coxe M, Hla KM, et al. Longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med 2006;166:1709-15. [Crossref] [PubMed]
- Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013;177:1006-14. [Crossref] [PubMed]
- Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 2015;3:310-8. [Crossref] [PubMed]
- Franklin KA, Sahlin C, Stenlund H, et al. Sleep apnoea is a common occurrence in females. Eur Respir J 2013;41:610-5. [Crossref] [PubMed]
- Tarasiuk A, Reuveni H. The economic impact of obstructive sleep apnea. Curr Opin Pulm Med 2013;19:639-44. [Crossref] [PubMed]
- Sung CM, Tan SN, Shin MH, et al. The Site of Airway Collapse in Sleep Apnea, Its Associations with Disease Severity and Obesity, and Implications for Mechanical Interventions. Am J Respir Crit Care Med 2021;204:103-6. [Crossref] [PubMed]
- Sanders AE, Essick GK, Fillingim R, et al. Sleep apnea symptoms and risk of temporomandibular disorder: OPPERA cohort. J Dent Res 2013;92:70S-77S. [Crossref] [PubMed]
- Mehra P, Nadershah M, Chigurupati R. Is Alloplastic Temporomandibular Joint Reconstruction a Viable Option in the Surgical Management of Adult Patients With Idiopathic Condylar Resorption? J Oral Maxillofac Surg 2016;74:2044-54. [Crossref] [PubMed]
- Mehra P, Downie M, Pita MC, et al. Pharyngeal airway space changes after counterclockwise rotation of the maxillomandibular complex. Am J Orthod Dentofacial Orthop 2001;120:154-9. [Crossref] [PubMed]
- Henry CH, Hughes CV, Gérard HC, et al. Reactive arthritis: preliminary microbiologic analysis of the human temporomandibular joint. J Oral Maxillofac Surg 2000;58:1137-42; discussion 1143-4. [Crossref] [PubMed]
- Van Damme PA, Merkx MA. Condylar resorption after orthognathic surgery. J Oral Maxillofac Surg 1994;52:1347-8. [Crossref] [PubMed]
- Gunson MJ, Arnett GW, Milam SB. Pathophysiology and pharmacologic control of osseous mandibular condylar resorption. J Oral Maxillofac Surg 2012;70:1918-34. [Crossref] [PubMed]
- Milam SB. Pathogenesis of degenerative temporomandibular joint arthritides. Odontology 2005;93:7-15. [Crossref] [PubMed]
- Alessandri-Bonetti A, Scarano E, Fiorita A, et al. Prevalence of signs and symptoms of temporo-mandibular disorder in patients with sleep apnea. Sleep Breath 2021;25:2001-6. [Crossref] [PubMed]
- Goodday RH, Bourque SE, Edwards PB. Objective and subjective outcomes following MMA surgery for treatment of patients with extremely severe obstructive sleep apnea (apnea-hypopnea index >100). J Oral Maxillofac Surg 2016;74:583-9. [Crossref] [PubMed]
- Mishima K, Yamada T, Sugahara T. Evaluation of respiratory status and mandibular movement after total temporomandibular joint replacement in patients with rheumatoid arthritis. Int J Oral Maxillofac Surg 2003;32:275-9. [Crossref] [PubMed]
- Gonçalves JR, Gomes LC, Vianna AP, et al. Airway space changes after maxillomandibular counterclockwise rotation and mandibular advancement with TMJ Concepts® total joint prostheses: three-dimensional assessment. Int J Oral Maxillofac Surg 2013;42:1014-22. [Crossref] [PubMed]
- Kim KB, Movahed R, Malhotra RK, et al. Maxillomandibular Advancement Using Total Joint Replacement for the Treatment of Obstructive Sleep Apnea. In Management of obstructive sleep apnea: An evidence-based, multidisciplinary textbook. Springer, 2021.
- Potter JK, Dierks EJ. Vascularized options for reconstruction of the mandibular condyle. Semin Plast Surg 2008;22:156-60. [Crossref] [PubMed]
- Coleta KE, Wolford LM, Goncalves JR, et al. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ Concepts total joint prostheses: part II airway changes and stability. Int J Oral Maxillofac Surg 2009;38:228e35.
- Smith MT, Wickwire EM, Grace EG, et al. Sleep disorders and their association with laboratory pain sensitivity in temporomandibular joint disorder. Sleep 2009;32:779-90. [Crossref] [PubMed]
- Paul SA, Simon SS, Issac B, et al. Management of severe sleep apnea secondary to juvenile arthritis with temporomandibular joint replacement and mandibular advancement. J Pharm Bioallied Sci 2015;7:S687-90. [Crossref] [PubMed]
- Dubrovsky B, Raphael KG, Lavigne GJ, et al. Polysomnographic investigation of sleep and respiratory parameters in women with temporomandibular pain disorders. J Clin Sleep Med 2014;10:195-201. [Crossref] [PubMed]
- Tay DKL, Pang KP. Clinical phenotype of South-East Asian temporomandibular disorder patients with upper airway resistance syndrome. J Oral Rehabil 2018;45:25-33. [Crossref] [PubMed]
- Kuo PC, West RA, Bloomquist DS, et al. The effect of mandibular osteotomy in three patients with hypersomnia sleep apnea. Oral Surg Oral Med Oral Pathol 1979;48:385-92. [Crossref] [PubMed]
- Riley RW, Powell NB, Guilleminault C, et al. Maxillary, mandibular, and hyoid advancement: an alternative to tracheostomy in obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg 1986;94:584-8. [Crossref] [PubMed]
- Zaghi S, Holty JE, Certal V, et al. Maxillomandibular Advancement for Treatment of Obstructive Sleep Apnea: A Meta-analysis. JAMA Otolaryngol Head Neck Surg 2016;142:58-66. [Crossref] [PubMed]
- Woods CM, Gunawardena I, Chia M, et al. Long-term quality-of-life outcomes following treatment for adult obstructive sleep apnoea: comparison of upper airway surgery, continuous positive airway pressure and mandibular advancement splints. Clin Otolaryngol 2016;41:762-70. [Crossref] [PubMed]
- Mercuri LG, Wolford LM, Sanders B, et al. Long-term follow-up of the CAD/CAM patient fitted total temporomandibular joint reconstruction system. J Oral Maxillofac Surg 2002;60:1440-8. [Crossref] [PubMed]
- Wolford LM, Mercuri LG, Schneiderman ED, et al. Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: the Techmedica/TMJ Concepts device. J Oral Maxillofac Surg 2015;73:952-60. [Crossref] [PubMed]
- Kezirian EJ. Nonresponders to pharyngeal surgery for obstructive sleep apnea: insights from drug-induced sleep endoscopy. Laryngoscope 2011;121:1320-6. [Crossref] [PubMed]
- Pirklbauer K, Russmueller G, Stiebellehner L, et al. Maxillomandibular advancement for treatment of obstructive sleep apnea syndrome: a systematic review. J Oral Maxillofac Surg 2011;69:e165-76. [Crossref] [PubMed]
- Li KK, Riley RW, Powell NB, et al. Patient's perception of the facial appearance after maxillomandibular advancement for obstructive sleep apnea syndrome. J Oral Maxillofac Surg 2001;59:377-80; discussion 380-1. [Crossref] [PubMed]
- Li KK, Powell NB, Riley RW, et al. Long-term results of maxillomandibular advancement surgery. Sleep Breath 2000;4:137-40. [Crossref] [PubMed]
- Bettega G, Pépin JL, Veale D, et al. Obstructive sleep apnea syndrome. fifty-one consecutive patients treated by maxillofacial surgery. Am J Respir Crit Care Med 2000;162:641-9. [Crossref] [PubMed]
- Greco JM, Frohberg U, Van Sickels JE. Cephalometric analysis of long-term airway space changes with maxillary osteotomies. Oral Surg Oral Med Oral Pathol 1990;70:552-4. [Crossref] [PubMed]
- Walker DA, Turvey TA, Warren DW. Alterations in nasal respiration and nasal airway size following superior repositioning of the maxilla. J Oral Maxillofac Surg 1988;46:276-81. [Crossref] [PubMed]
- Guenthner TA, Sather AH, Kern EB. The effect of Le Fort I maxillary impaction on nasal airway resistance. Am J Orthod 1984;85:308-15. [Crossref] [PubMed]
- Yu CC, Hsiao HD, Tseng TI, et al. Computational fluid dynamics study of the inspiratory upper airway and clinical severity of obstructive sleep apnea. J Craniofac Surg 2012;23:401-5. [Crossref] [PubMed]
- Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion--idiopathic condylar resorption. Part I. Am J Orthod Dentofacial Orthop 1996;110:8-15. [Crossref] [PubMed]
- Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion-idiopathic condylar resorption. Part II. Am J Orthod Dentofacial Orthop 1996;110:117-27. [Crossref] [PubMed]
- Mercuri LG. A rationale for total alloplastic temporomandibular joint reconstruction in the management of idiopathic/progressive condylar resorption. J Oral Maxillofac Surg 2007;65:1600-9. [Crossref] [PubMed]
- Wolford LM. Clinical indications for simultaneous TMJ and orthognathic surgery. Cranio 2007;25:273-82. [Crossref] [PubMed]
- Perez DE, Wolford LM, Schneiderman E, et al. Does Unilateral Temporomandibular Total Joint Reconstruction Result in Contralateral Joint Pain and Dysfunction? J Oral Maxillofac Surg 2016;74:1539-47. [Crossref] [PubMed]
- Mercuri LG. Patient-fitted ("custom") alloplastic temporomandibular joint replacement technique. Atlas Oral Maxillofac Surg Clin North Am 2011;19:233-42. [Crossref] [PubMed]
- Granquist EJ, Quinn PD. Total reconstruction of the temporomandibular joint with a stock prosthesis. Atlas Oral Maxillofac Surg Clin North Am 2011;19:221-32. [Crossref] [PubMed]
- Abramowicz S, Barbick M, Rose SP, et al. Adaptability of stock TMJ prosthesis to joints that were previously treated with custom joint prosthesis. Int J Oral Maxillofac Surg 2012;41:518-20. [Crossref] [PubMed]
- Movahed R, Teschke M, Wolford LM. Protocol for concomitant temporomandibular joint custom-fitted total joint reconstruction and orthognathic surgery utilizing computer-assisted surgical simulation. J Oral Maxillofac Surg 2013;71:2123-9. [Crossref] [PubMed]
- Yang L, Sun Y, Li G, et al. Is hemoglobin A1c and perioperative hyperglycemia predictive of periprosthetic joint infection following total joint arthroplasty?: A systematic review and meta-analysis. Medicine (Baltimore) 2017;96:e8805. [Crossref] [PubMed]
- Green JM 3rd, Lawson ST, Liacouras PC, et al. Custom Anatomical 3D Spacer for Temporomandibular Joint Resection and Reconstruction. Craniomaxillofac Trauma Reconstr 2016;9:82-7. [Crossref] [PubMed]
- Olate S, Unibazo A, Almeida A, et al. Mandibular condylectomy revisited: technical notes concerning the use of an ultrasonic system. J Oral Maxillofac Surg 2014;72:481-4. [Crossref] [PubMed]
- Mercuri LG, Ali FA, Woolson R. Outcomes of total alloplastic replacement with periarticular autogenous fat grafting for management of reankylosis of the temporomandibular joint. J Oral Maxillofac Surg 2008;66:1794-803. [Crossref] [PubMed]
- Wolford LM, Morales-Ryan CA, Morales PG, et al. Autologous fat grafts placed around temporomandibular joint total joint prostheses to prevent heterotopic bone formation. Proc (Bayl Univ Med Cent) 2008;21:248-54. [Crossref] [PubMed]
- Wolford LM, Karras SC. Autologous fat transplantation around temporomandibular joint total joint prostheses: preliminary treatment outcomes. J Oral Maxillofac Surg 1997;55:245-51; discussion 251-2. [Crossref] [PubMed]
Cite this article as: Movahed R, Semensohn R. Indications for alloplastic total joint replacement in obstructive sleep apnea patients requiring maxillomandibular advancement. Front Oral Maxillofac Med 2023;5:38.

