
Suggestions on management process of throat pack in orthognathic surgery: a case report and literature review
Highlight box
Key findings
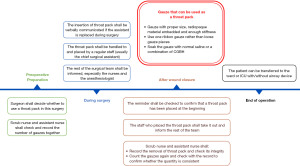
• This article reported a specific and operable management process for using a throat pack in orthognathic surgery.
What is known and what is new?
• Many precautions of missing throat pack have been proposed in different literatures, yet the suggestions are too scattered and lack of standardized processes. This article summarized the clinical experience in the literature and our center, and formulated a standardized process whose reliability has been proven by our years of practice.
What is the implication, and what should change now?
• The risks of using a throat pack in orthognathic surgery must be realized, and the necessity should be carefully evaluated before surgery. The implementation of a standardized process helps to avoid accidents and reduce risks.
Introduction
Throat packs (TPs), also known as surgical gauzes, pharyngeal packs or gauze packs, are commonly employed as a physical barrier in general anesthesia surgeries to prevent accidental aspiration or ingestion of fragments, blood and instruments. However, the retention of TP can cause serious complications and may even lead to fatal consequences (1-3). Although considered as one of the Never Events which refers to those incidents that are believed to be preventable with appropriate measures (4,5), retained TPs occurred eight times in 2013–2014 and 2014–2015 and five times in 2015–2016 (6). In this article, we reported an orthognathic surgery during which the TP was missing and found back. Based on this case and literature review, we summarized the causes and countermeasures of missing TP in orthognathic surgery, and proposed a standardized process and a coping strategy to retrieve a missing TP. We present the following case in accordance with the CARE reporting checklist (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-30/rc).
Case presentation
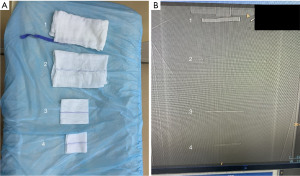
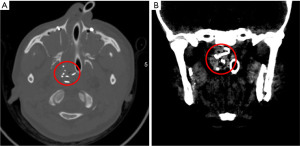
A 26-year-old female patient underwent bimaxillary surgery for skeletal Class III malocclusion under general anesthesia and nasotracheal intubation. The brackets were counted and a 7.5 cm × 7.5 cm gauze with radiopaque wire was placed in the pharynx by an assistant. Others in the operating room were informed, including the surgeon, other assistants, anesthesiologists, and nurses. On the white board the note “Throat Pack In” was written by assistant nurse right after its placement. The surgery went smooth. The patient awoke and swallowed once during suturing. After wound closure, the gauze was not found in patient’s pharynx. The scrub nurse and assistant nurse checked the note on the white board and the number of gauzes together, and confirmed that the TP had not been removed during surgery. Fiberoptic bronchoscopy was applied to inspect the oropharynx, airway and esophagus, yet no gauze was found. Meanwhile, scrub nurse, assistant nurse and the chief nurse sorted and counted the gauzes several times and reconfirmed that TP was not taken out. The gauze was developed neither in the patient’s body nor next to the patient’s head where a gauze from the same package was placed for reference on C-arm X-ray image (Figure 1). Considering that it might be caused by the low-resolution ratio of X-ray, or the poor quality of the radiopaque components in these gauzes, computed tomography (CT) scan was decided to be performed immediately. Firstly, the radiopaque components were well displayed in CT images with 1mm slice thickness (SOMATOM Definition Flash, Siemens Healthineers, Forchheim, Germany) (Figure 2). Then, well defined high-density images were viewed in the right nasopharynx on maxillofacial CT (Figure 3). The patient was shifted back to the operation room. After re-disinfection, the TP was taken out with forceps successfully (Figure 4). The patient was then transferred to intensive care unit (ICU) for routine monitoring overnight and was extubated smoothly the next day. The rest of her recovery was uneventful.

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Literature review
Database of PubMed, Web of Knowledge and China National Knowledge Infrastructure (CNKI) were searched independently using the search terms: (((throat pack) OR (surgical gauze)) OR (pharyngeal pack)) OR (gauze pack). Reviews, case reports and clinical studies were all included. The last search was updated on 4 August 2022. The search process was conducted by the first author, and titles and abstracts were screened by two reviewers and potentially eligible articles were read through to assess their relevance.
Discussion
TPs are widely used in ear, nose and throat, oral and dental surgery to prevent aspiration or ingestion of blood and surgical debris, and to avoid displacement of the artificial airway device (7). They were also thought profitable in alleviating postoperative nausea and vomiting (PONV). However, many recent research has pointed out that the usage of TP had little benefit in reducing PONV, but was instead associated with worse sore throats and postoperative dysphagia (8-10). A randomized, controlled research has confirmed it as a predisposing factor for postoperative aphthous stomatitis (11). Although in two studies the TP soaked with a combination of chlorhexidine gluconate and benzydamine hydrochloride (CGBH) was used to reduce sore throats, the difference did not reach statistical significance (12,13). Therefore, using TP to alleviate PONV was not recommended. As a regular means to prevent accidental aspiration and ingestion, the merits of TP are rarely discussed in the article. After all, the incidence of these complications is itself very low. But this does not mean that this method is not beneficial. For orthognathic patients who have isolated brackets and attachments in their mouths, the placement of TP is still a low-cost, simple and effective measure.
However, a forgotten TP could lead to airway obstruction, foreign body in vivo and postoperative infection. Many cases of missing TPs have been reported in earlier literature (14-18). Ninety-three (38.27%) Indian anesthesiologists participated in a nationwide survey had encountered retained TP which led to airway obstruction in 37.6% cases (19), while 42 respondents of a national survey in the UK reported 52 critical incidents of retained TP (2). In some cases, the missing TP was found and retrieved soon after the surgery, under endoscopy or vomited out by the patient. Muñoz and Villafruela reported a case in which the forgotten gauze had been left in a 6-year-old boy for 3 weeks before removed (18). In a case reported by Ozer et al. the gauze was removed 6mo after adenotonsillectomy, causing the patient’s purulent rhinorrhea, nasal obstruction, halitosis, and mouth breathing after surgery (14). The accidental ingestion of TP has not only happened in general anesthesia surgeries, but also local anesthesia surgeries. A 66-year-old woman swallowed the TP without notice during an endoscopic dacryocystorhinostomy (en-DCR) (20).
The common causes of a forgotten TP may include, but are not limited to, the following:
- Putting a TP without informing other staff, or the shift of crew.
- Putting a TP without a visual reminder.
- Extubating before doing the final gauze count;
- False statement that the TP has been removed;
- More TPs placed than removed, or a torn TP.
In order to avoid a retained TP, a couple of aspects are important to note here:
- Type of surgery: a consensus should be reached on which type of surgery or patient shall use a TP. For example, patients with orthodontic devices, loosen teeth or bone fragments, or those who need small, easily broken instruments during surgery. Anesthesiologists and surgical nurses collaborate with different doctors every day. A clear consensus let them know under what circumstances a TP will be used, so that they can remind doctors to remove it when necessary.
- Person in charge:
a regular staff should be assigned to place and take out the TP. Otherwise, everyone may think that someone else will place the TP, or, conversely, multiple TPs may be put by more than one person. In our center, the task is usually done by the chief surgical assistant because he/she usually participates in the whole process of the surgery and is not subbed. If the assistant needs to be changed, it must be verbally communicated whether a TP has been placed. - Teamwork: all medical staff in the operating room should be informed when the TP is placed, especially the nurses and the anesthesiologist. The surgeons need to check the number of brackets and attachment, and the scrub nurse and assistant nurse need to check the number of gauzes together before and after surgery. The incisions of orthognathic surgery are usually too small to accommodate TP, therefore the gauze count can be done after wound closure. In other oral surgeries, such as oral tumor resection, the gauzes should be checked before suturing. The anesthesiologist needs to check the pharyngeal cavity for foreign bodies before extubation, and the patient must not be extubated before the TP is confirmed.
- Visual reminder: at least one visual reminder should be made when the TP is placed, such as a mark on patient’s face, a tab on the airway device, or a label attached to the surgical assistant’s hat (21). In our center, a reminder is always written on the white board by assistant nurse, and will be erased the only after he/she see the removed TP after surgery. Some articles suggest leaving part of the TP protruding externally, but the external end would interfere with the occlusion, which makes this method not applicable in orthognathic surgery.
- Type of gauze: only one gauze with proper size, radiopaque material embedded and enough stiffness can be used as the TP. We recommend to use a 10 cm × 10 cm gauze soaked with normal saline or CGBH, because an oversized gauze or a dry gauze will increase the risk of sore throats and postoperative ulcers. Small gauze pieces are not easy to be found (just like the TP in our case), and have higher risk of being left in the incisions. Using loose gauze pieces or a fragile gauze will make it hard to find out if there are any pieces left. A gauze without radiopaque material embedded cannot be seen on X-ray or CT, therefore, the patient will have to undergo invasive examination such as an endoscopy to look for the missing TP.
- Coping strategy: if the TP is missing during surgery, its location must be determined immediately. Visual reminder and the number of gauzes should be checked to make sure whether a TP has been placed. Fiberoptic bronchoscopy can be used to inspect nasopharynx and oropharynx, and then X-ray or CT for further inspection if necessary. In patient with intraoral brackets, CT in maxillofacial region is recommended because the metal artifact will make the TP difficult to distinguish on X-ray. The TP should be retrieved under direct visualization or endoscope once it is found because it would not go too deep in a short period. The most important thing to prevent accidental aspiration or ingestion is that the patient can be extubated only after confirming that the TP is taken.
Conclusions
In this case, we showed a management process of missing TP during orthognathic surgery, similar to but more specific and operable than the existing recommendations (6) (Figure 5). One reason for this case was that the gauze used as TP was too small, and the patient’s awakening and gulp made us mistakenly think that the gauze was swallowed, neglecting the examination of nasopharynx. It was precisely because of such a standardized process that the missing TP could be retrieved immediately without serious consequences. It must be admitted that the use of TP has certain risks, and its indication and necessity should be carefully evaluated before surgery. The most important thing to prevent serious complications is not to do the extubation before the missing TP is found and retrieved.
Acknowledgments
Funding: This work was supported by the Clinical Research Program of 9th People’s Hospital affiliated to Shanghai Jiao Tong University School of Medicine (Grant No. JYLJ202001).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-30/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-30/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Crawford BS. Prevention of retained throat pack. Br Med J 1977;2:1029. [Crossref] [PubMed]
- Knepil GJ, Blackburn CW. Retained throat packs: results of a national survey and the application of an organisational accident model. Br J Oral Maxillofac Surg 2008;46:473-6. [Crossref] [PubMed]
- Smarius BJA, Guillaume CHAL, Jonker G, et al. The use of throat packs in pediatric cleft lip/palate surgery: a retrospective study. Clin Oral Investig 2018;22:3053-9. [Crossref] [PubMed]
- Moppett IK, Moppett SH. Surgical caseload and the risk of surgical Never Events in England. Anaesthesia 2016;71:17-30. [Crossref] [PubMed]
- Pandit JJ. Deaths by horsekick in the Prussian army - and other 'Never Events' in large organisations. Anaesthesia 2016;71:7-11. [Crossref] [PubMed]
- Athanassoglou V, Patel A, McGuire B, et al. Systematic review of benefits or harms of routine anaesthetist-inserted throat packs in adults: practice recommendations for inserting and counting throat packs: An evidence-based consensus statement by the Difficult Airway Society (DAS), the British Association of Oral and Maxillofacial Surgery (BAOMS) and the British Association of Otorhinolaryngology, Head and Neck Surgery (ENT-UK). Anaesthesia 2018;73:612-8. [Crossref] [PubMed]
- Smith M, Turnbull D, Andrzejowski J. Throat packs in neuroanaesthesia. Anaesthesia 2012;67:804-5. [Crossref] [PubMed]
- Jin HJ, Kim S, Hwang SH. Can Pharyngeal Packing Prevent Postoperative Nausea and Vomiting in Nasal Surgery? Laryngoscope 2019;129:291-8. [Crossref] [PubMed]
- Faro TF, de Oliveira E, Silva ED, Campos GJ, et al. Effects of throat packs during orthognathic surgery: a double-blind randomized controlled clinical trial. Int J Oral Maxillofac Surg 2021;50:349-55. [Crossref] [PubMed]
- Anderson CR, Premakumar Y, Navaratnam AV, et al. The use of throat packs in ear, nose and throat, oral and dental surgery: a systematic review. Rhinology 2020;58:306-13. [Crossref] [PubMed]
- Erkalp K, Korkut YA, Meric A, et al. Pharyngeal packing is a predisposing factor for postoperative aphthous stomatitis in nasal surgery. Otolaryngol Head Neck Surg 2010;142:672-6. [Crossref] [PubMed]
- Vural Ç, Yurttutan ME, Sancak KT, et al. Effect of chlorhexidine/benzydamine soaked pharyngeal packing on throat pain and postoperative nausea & vomiting in orthognathic surgery. J Craniomaxillofac Surg 2019;47:1861-7. [Crossref] [PubMed]
- Meco BC, Ozcelik M, Yildirim Guclu C, et al. Does Type of Pharyngeal Packing during Sinonasal Surgery Have an Effect on PONV and Throat Pain? Otolaryngol Head Neck Surg 2016;154:742-7. [Crossref] [PubMed]
- Ozer C, Ozer F, Sener M, et al. A forgotten gauze pack in the nasopharynx: an unfortunate complication of adenotonsillectomy. Am J Otolaryngol 2007;28:191-3. [Crossref] [PubMed]
- To EW, Tsang WM, Yiu F, et al. A missing throat pack. Anaesthesia 2001;56:383-4. [Crossref] [PubMed]
- Iwai T, Goto T, Matsui Y, et al. Endoscopic removal of throat-packing gauze swallowed during general anesthesia. J Craniofac Surg 2012;23:1547-9. [Crossref] [PubMed]
- Basha MS. Missing Pharyngeal Pack Endoscopically Retrieved: An Avoidable Complication. Ann Maxillofac Surg 2018;8:342-3. [Crossref] [PubMed]
- Muñoz A, Villafruela M. MR imaging recognition of nasopharyngeal gauze retention in a child. Pediatr Radiol 2000;30:811-2. [Crossref] [PubMed]
- Gupta A, Sarma R, Gupta N, et al. Current practices and beliefs regarding the use of oropharyngeal throat pack in India: A nationwide survey. Indian J Anaesth 2021;65:241-7. [Crossref] [PubMed]
- Kitaguchi Y, Mupas-Uy J, Takahashi Y, et al. Accidental Ingestion of Nasal Packing Gauze during Endonasal Endoscopic Dacryocystorhinostomy under Local Anesthesia: A Case Report. Case Rep Ophthalmol 2017;8:31-4. [Crossref] [PubMed]
- Jennings A, Bhatt V. Throat packs: in your face? Anaesthesia 2010;65:312-3. [Crossref] [PubMed]


