The versatility of Bio-Oss® Collagen in orthognathic surgery: two case reports from vertical chin augmentation to pseudoarthrosis treatment
Introduction
Orthognathic surgery is a procedure aesthetic-functional that aims to correct dentofacial deformities by repositioning the maxillary bones in relation to the skull base. Numerous techniques have already been described, aiming at improving the procedure, with the intention of reducing morbidity and the operative time (1-4). With the advancement of fixation techniques and materials, there has been greater safety and predictability in the resolution of complex cases, but there are always risks of possible complications, such as pseudoarthrosis and non-union between the segmented bones. Instability between the bone bases, inadequate bone contact or even the failure of the osteosynthesis material, can lead to a failure of the proposed surgical treatment, which can lead to both a functional problem and an aesthetic breakdown (5). In addition, resorption and bone defects resulting from the formation of pseudoarthrosis in osteotomy lines, may generate the need for immediate correction through the use of autogenous bone grafts or biomaterials with slow absorption on the local (6).
The bone repair process of the osteotomy lines in orthognathic surgery occurs with the same biological bases as the consolidation of any bone fracture. Osteotomies can be considered as fractures with displacements previously planned to remain in contact of the two segments, the fixed and the displaced, however, if this displacement is not well planned or performed during the bone fixation process, it can lead to an insufficient area of bone contact to occur its stability, and thus, the beginning of the formation of angiogenesis, which is essential for the formation of the bone repair process, may be compromised. The delay or interruption of angiogenesis can totally compromise the repair process leading to pseudoarthrosis and non-union. In some surgical movements, such as in the lower repositioning of the maxilla or chin, where this type of movement generates a gap between the two osteotomized bone segments, the repair process may be called gap healing, and in these cases, the stability of the bone segments is essential for this space to remain without displacement during the process of chewing, swallowing and speaking (7,8). The use of grafting in these regions helps in the stability of bone bases and in the repair process, decreasing the chances of pseudoarthrosis and non-union, leading to long-term repair stability (9,10).
The use of Bio-Oss® Collagen as the first choice grafting material in these types of displacement mentioned above has the advantage of not requiring a donor area for graft collection, less surgical time and greater stability of the grafted bone volume in the long term when compared to particulate autogenous graft. As the particle of this material has slow degradation, it provides the graft with the property of bone osteoconduction and the maintenance of the grafted volume (9). In a study by Jensen using some proportions of Bio-Oss® mixed with particulate autogenous bone to maintain bone volume in a maxillary sinus survey, it was possible to verify greater volume maintenance when the biomaterial was used without mixing with autogenous bone (11).
When the collagen was incorporated into the Bio-Oss® particle, its manipulation became easier thanks to the collagen property of greater adhesion to the walls of the residual bone tissue and the maintenance of its shape in large or small defects. This material can also be used in different specialties such as in Traumatology, Implantology and Periodontics (9,12-14). The main indication of the material is alveolar preservation, but it can also be used to increase and reconstruct the alveolar process, interpositional material in gaps, filler of bone defects, lifting of the maxillary sinus, support for the membrane during guided bone regeneration (GBR) and even guided tissue regeneration (GTR) (14).
In exophytic use in bone grafting and reconstruction, Bio-Oss® Collagen showed good bone volume maintenance and the morphological characteristic of the bone pattern was similar to trabecular bone type III to IV, with the presence of bone neoformation mainly in the peripheries of the grafted area (15). This type of modeling of biomaterial greatly favors its indication in filling small gaps and small areas that need stability complementary to that of the fixation system, however more studies are needed to assess what are the space and stability limitations provided by the material used alone, or accompanied by the fixation system for these purposes. We present the following article in accordance with the CARE reporting checklist (available at https://fomm.amegroups.com/article/view/10.21037/fomm-21-37/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from both patients for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Case 1—vertical chin increase
Female patient, 49 years old, with Class II type malocclusion, attended the private clinic with complaints of: malocclusion and short face. Based on the facial analysis described by Arnett G. and collaborators in 1999, it was found that the patient’s maxillary height was within the facial standards, while the mandibular height was below ideal (31.0 mm), which justified the patient’s complaint (16) (Figure 1). Associating the clinical analysis to the image exam, the following planning was carried out:
- 5.5 mm mandibular advancement, without alteration of the occlusal plane;
- Mentoplasty with vertical movement, increasing 3.0 mm.
The major challenge in this case would be to maintain the stability of the chin height, as this type of movement forms a major defect that could easily become a pseudoarthrosis.
The procedure started with bilateral sagittal osteotomy of the mandible with the Lingual Short Split technique (4), which ensured adequate bone contact followed by the fixation of the stumps through the hybrid fixation technique (17), which promoted stability and maintenance of the spaces between the stumps proximal and medial. After completion of the mandible advancement, infiltration was performed in the groove fundus region of the chin with 2% Xylocaine with vasoconstrictor. The technique begins with a 1.0 cm incision after the bottom of the groove in the region between the lower canines, proceeding towards the bone tissue. Total detachment is performed and the midline of the chin is marked with a 702 carbide drill mounted on a straight multiplier part. With a reciprocating saw, osteotomy was performed in the lateral-lateral direction until the corticals ruptured (Figure 2). After repositioning the chin at the planned height, fixation was performed with 3 plates of the 2.0 system, which reinforced the stability of the bone base in the position (Figure 3). After placing the osteosynthesis material, the gap with 500 mg Bio-Oss® Collagen, condensing the material firmly, so that no space would form in this region (Figure 4).

After filling the region with biomaterial, the tissues were synthesized with Vicryl® 3-0 and Vicryl® 4-0. No unexpected events occurred during the procedure. The patient is in 2-year postoperative control and it was possible to observe that in addition to the gain in height of the chin, from 31.0 to 39.0 mm, there was also a change in the contour of the mental region, leaving the face more harmonious (Figure 5).
Case 2—pseudoarthrosis after orthognathic surgery
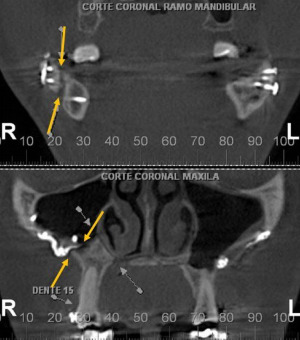
Female patient, 33 years old, attended the private clinic complaining of dissatisfaction with the result of previous orthognathic surgery performed in another service. He also reported episodes of discomfort in the jaw on the right side with unstable occlusion on the same side when he performed laterality and protrusion movements. During the physical examination, it was possible to observe instability of the maxilla and mandible, however, stability of the occlusion. With the aid of computed tomography, it was possible to make the diagnosis of pseudoarthrosis of the maxilla and mandible on the right side with severe displacement (Figure 6). As already discussed at the beginning of the article, one of the hypotheses of the etiology is the failure of the fixation material and/or the failure to fix the screws in the osteotomized stumps.
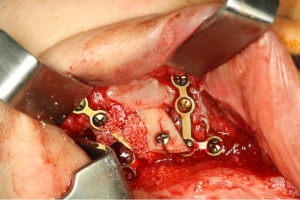
Then, a surgical reintervention was proposed for the patient in the regions where they presented pseudoarthrosis. Surgical access to the maxilla was 1.0 cm from the bottom of the groove, up to the region of the osteosynthesis material. This material was removed followed by curettage of the granulation tissue that was in place. A new osteosynthesis material was placed for the stable fixation of the stumps, however the space between them was subject to mobility due to the masticatory movements that the patient would perform in the postoperative period, so blocks of autogenous bone graft from the mental region were used to complete the maxillary gap associated with the Bio-Oss® Block, aiming at helping bone stabilization (Figure 7).
Mandibular surgery was performed with a 1.0 cm access at the bottom of the groove, extending from the retromolar region to the lower premolars. After total detachment, it was possible to locate the osteosynthesis material present there, which was removed and associated with curettage of the granulation tissue (Figure 8). Due to the difficulty of accessing this location, the adaptation of block-shaped grafts is more difficult, so we opted for the use of Bio-Oss® Collagen, filling not only the gap, but also improving the contour of the region where had pseudoarthrosis. No unexpected events occurred during the procedure.
The patient is in 4-year postoperative control, with stable occlusion, with no pain or complaints. In the tomographic examination, it is possible to observe the density of the newly formed bone and the osteosynthesis material still present, since it is of slow resorption.
Discussion
Orthognathic surgery is a procedure that should promote aesthetic and functional improvement to patients. In general, it is considered an elective surgery, since the patient needs preoperative preparation and not an emergency procedure, therefore, the acceptance of complications in the postoperative period by patients is not so simple, even if they are oriented about the risks of surgery.
The concern with the stability of orthognathic surgeries is not recent. Araújo and collaborators (18), in 1978, already studied hydroxyapatite-based grafts as a way to promote greater predictability of major surgical movements. They evaluated the recurrences of patients who underwent Le Fort I osteotomies and concluded that, in patients who used grafts for movement stability, they had a significantly lower recurrence.
In case 2 previously described, it was possible to observe the absence of contact between the bone bases, this being the probable cause of the pseudoarthrosis, therefore the gap region was debrided and refixed, placing osteosynthesis material from the 2.0 system, associated with the block that hydroxyapatite, promoting hemi-maxilla stability. The study carried out by Rohner et al. in 2013, showed that in patients submitted to Le Fort I osteotomy with advances of 5.0 mm or less, one side grafted with Bio-Oss® Collagen and the other side as a control, obtained after 6 months, all grafted sites repaired without defect, while three of the sites in the control group had a failure in the repair process, that is, even with the collagen associated with hydroxyapatite, it promoted a higher success rate (12).
The use of hydroxyapatite in surgeries is a long-standing one. In 1986, Kent et al. studied the indications for the use of hydroxyapatite isolated and associated with collagen and tested the most diverse surgical situations, such as: movements of rotation of the jaw; advance and rotations between the stumps of the mandible (19); defects in the regions of osteotomies in the mandible; and gain in height or width of the chin. During this study, the success rate for gain in height of the chin was 100%, which justifies the technique adopted in case 1. The association with collagen facilitates the adaptation of the biomaterial in the surgical gap, but it has already been proven that collagen alone does not induce bone formation. Its association with a biomaterial, promotes greater osteoconductivity than a material without an associated collagen matrix. In addition, its better adaptation in the surgical bed due to its malleability, promotes greater stabilization of the graft particles, facilitating the formation of a structured clot, which promotes an acceleration in the osteoblastic activity of the region (20). Therefore, the use of this biomaterial in regions of pseudoarthrosis, as shown in case 2, can increase the stability of osteotomies and help in modeling the patient’s bone contour. A similar case was carried out by Faria and collaborators, in 2020, who used the same material as an aid in the treatment of pseudoarthrosis after sagittal jaw osteotomy and obtained stable results of movement and facial profile (21).
Still in the study by Kent [1986], stability was analyzed in relation to mandibular advancement and rotations between the stumps, it was observed that advances above 6.0 mm, had difficulty maintaining stability due to the limitation of bone contact between the stumps, however, this problem was solved with the evolution of osteotomy and osteosynthesis techniques, since at the time these resources were still limited and the use of steel wire as a form of osteosynthesis favored pseudoarthrosis (19). Therefore, in treatments such as case 2, in which the defect was greater than 6.0 mm, the use of grafts is indicated. It is worth mentioning that the use of the hybrid technique of fixation of the sagittal osteotomy of the mandible using bicortical screws, associated with the plates with monocortical screws, is also a factor that reduces the risks of pseudoarthrosis. This is due to the bicortical screws promoting the maintenance of the space between the stumps and the plate maintaining the antero-posterior relationship (4).
According to Ferri et al. [2019], the most common complication found in orthognathic surgery is infection (22). Pseudoarthrosis and non-union are as rare as skull base fractures, representing only 0.19% of the cases in a survey of 5,025 cases. This reveals that great advances must be accompanied by good fixation practices, the correct choice of synthesis material and the indication of bone grafts associated with biomaterials for the stabilization of the stump displaced by the surgery, avoiding the formation of problems in the repair process of the lines. osteotomy.
Conclusions
Pseudoarthrosis and non-union, even though they are rare, are a challenge in the life of the maxillofacial surgeon. The stability between the osteotomized stumps is fundamental for the success of the repair process, therefore, the use of osteotomy techniques and adequate osteosynthesis, associated with the grafts can minimize complications and promote less morbidity in the surgical procedure.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Valfrido Antônio Pereira-Filho and Pedro Carvalho) for the series “Xenogenous and Xeno-synthetic Bone Substitutes: State-of-the-art and Clinical Outcomes” published in Frontiers of Oral and Maxillofacial Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://fomm.amegroups.com/article/view/10.21037/fomm-21-37/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-21-37/coif). The series “Xenogenous and Xeno-synthetic Bone Substitutes: State-of-the-art and Clinical Outcomes” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from both patients for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Caldwell JB, Letterman GS. Vertical osteotomy in the mandibular raml for correction of prognathism. J Oral Surg (Chic) 1954;12:185-202. [PubMed]
- Trauner R, Obwegeser H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg Oral Med Oral Pathol 1957;10:677-89. contd. [Crossref] [PubMed]
- Gotte P. On the surgical therapy of prognathism. Experiences and results of a modification of Obwegeser's intraoral method. Minerva Stomatol 1966;15:12-7. [PubMed]
- Sant'Ana E, Souza DPE, Temprano AB, et al. Lingual Short Split: A Bilateral Sagittal Split Osteotomy Technique Modification. J Craniofac Surg 2017;28:1852-4. [Crossref] [PubMed]
- Baker DL, Stoelinga PJ, Blijdorp PA, et al. Long-term stability after inferior maxillary repositioning by miniplate fixation. Int J Oral Maxillofac Surg 1992;21:320-6. [Crossref] [PubMed]
- Lindquist CC, Obeid G. Complications of genioplasty done alone or in combination with sagittal split-ramus osteotomy. Oral Surg Oral Med Oral Pathol 1988;66:13-6. [Crossref] [PubMed]
- Alyahya A, Swennen GRJ. Bone grafting in orthognathic surgery: a systematic review. Int J Oral Maxillofac Surg 2019;48:322-31. [Crossref] [PubMed]
- Joss CU, Vassalli IM. Stability after bilateral sagittal split osteotomy advancement surgery with rigid internal fixation: a systematic review. J Oral Maxillofac Surg 2009;67:301-13. [Crossref] [PubMed]
- Trevisiol L, Nocini PF, Albanese M, et al. Grafting of large mandibular advancement with a collagen-coated bovine bone (Bio-Oss Collagen) in orthognathic surgery. J Craniofac Surg 2012;23:1343-8. [Crossref] [PubMed]
- Stetzer K, Cooper G, Gassner R, et al. Effects of fixation type and guided tissue regeneration on maxillary osteotomy healing in rabbits. J Oral Maxillofac Surg 2002;60:427-36; discussion 436-7. [Crossref] [PubMed]
- Jensen T, Schou S, Stavropoulos A, et al. Maxillary sinus floor augmentation with Bio-Oss or Bio-Oss mixed with autogenous bone as graft: a systematic review. Clin Oral Implants Res 2012;23:263-73. [Crossref] [PubMed]
- Rohner D, Hailemariam S, Hammer B. Le Fort I osteotomies using Bio-Oss® collagen to promote bony union: a prospective clinical split-mouth study. Int J Oral Maxillofac Surg 2013;42:585-91. [Crossref] [PubMed]
- Araújo MG, Liljenberg B, Lindhe J. Dynamics of Bio-Oss Collagen incorporation in fresh extraction wounds: an experimental study in the dog. Clin Oral Implants Res 2010;21:55-64. [Crossref] [PubMed]
- Mordenfeld A, Albrektsson T, Hallman M. A 10-year clinical and radiographic study of implants placed after maxillary sinus floor augmentation with an 80:20 mixture of deproteinized bovine bone and autogenous bone. Clin Implant Dent Relat Res 2014;16:435-46. [Crossref] [PubMed]
- Borges CD, Faria PEP, Pessôa de Oliveira PGF, et al. Influence of collagen membrane on bone quality in titanium mesh reconstructions-Study in rats. J Periodontol 2020;91:1673-81. [Crossref] [PubMed]
- Arnett GW, Jelic JS, Kim J, et al. Soft tissue cephalometric analysis: diagnosis and treatment planning of dentofacial deformity. Am J Orthod Dentofacial Orthop 1999;116:239-53. [Crossref] [PubMed]
- Pereira FL, Janson M, Sant'Ana E. Hybrid fixation in the bilateral sagittal split osteotomy for lower jaw advancement. J Appl Oral Sci 2010;18:92-9. [Crossref] [PubMed]
- Araujo A, Schendel SA, Wolford LM, et al. Total maxillary advancement with and without bone grafting. J Oral Surg 1978;36:849-58. [PubMed]
- Kent JN, Zide MF, Kay JF, et al. Hydroxylapatite blocks and particles as bone graft substitutes in orthognathic and reconstructive surgery. J Oral Maxillofac Surg 1986;44:597-605. [Crossref] [PubMed]
- Jambhekar S, Kernen F, Bidra AS. Clinical and histologic outcomes of socket grafting after flapless tooth extraction: a systematic review of randomized controlled clinical trials. J Prosthet Dent 2015;113:371-82. [Crossref] [PubMed]
- Faria PEP, Chihara LL, Sakima V, et al. Treatment of Nonunion in the Mandible After Orthognathic Surgery to Correct Transverse Asymmetry of the Face. Craniomaxillofacial Trauma & Reconstruction Open 2020;5:1-8. [Crossref]
- Ferri J, Druelle C, Schlund M, et al. Complications in orthognathic surgery: A retrospective study of 5025 cases. Int Orthod 2019;17:789-98. [Crossref] [PubMed]
Cite this article as: Chihara LL, De Marco R, Faria PEP, Sant’Ana E. The versatility of Bio-Oss® Collagen in orthognathic surgery: two case reports from vertical chin augmentation to pseudoarthrosis treatment. Front Oral Maxillofac Med 2023;5:30.