
Rehabilitation with implants succeeding conservative management of odontogenic keratocyst: a case report with a 6-year follow-up and literature review
Highlight box
Key findings
• Complete regression of the lesion with no signs of recurrence with Decompression technique.
• Novel technique to asses quality of bone using cone-beam computed tomography.
• Rehabilitation of missing tooth using dental implant in the regenerated bone.
What is known and what is new?
• Conservative treatment modalities in the management of odontogenic keratocyst (OKC).
• Extensive OKC involving the ramus and body of the mandible treated with decompression and Enucleation. A novel method is presented to evaluate bone density using cone beam computed tomography from the surgeon’s perspective for rehabilitation using a dental implant.
What is the implication, and what should change now?
• The cited case emphasizes the significance of patient compliance and long term follow up for successful treatment in cases managed with conservative modalities.
• Radical methods to be preserved only for cases of multiple recurrence and extremes of age.
Introduction
Management of odontogenic keratocyst (OKC) involving jaw bones has evolved over time, from radical methods to conservative modalities. Even though it has been reported in the literature that more aggressive treatment modalities such as resection are associated with the lowest recurrence rates (0%), conservative treatments like decompression followed by enucleation or curettage complemented with the application of Carnoy’s solution (7.8%) and cryotherapy (11.5%) are widely used (1). Conservative treatment not only preserves the jaw bones but also allows functional rehabilitation, which contributes to the overall psychological well-being of the patient.
OKC is well known for causing extensive destruction of medullary bone with minimal buccolingual expansion by the time it is diagnosed. Because of its odontogenic origin and rapid widespread bone destruction, the treatment typically includes not only the removal of the entire pathological lining but may also necessitate extraction of multiple teeth involved in the lesion (2). Owing to the high recurrence potential (16–30%), extensive periodic follow-up is required (2). Following complete resolution of the pathology, functional rehabilitation of alveolar bone and teeth remains a challenge. Depending on the size of the residual bony defect, regeneration can be left to occur spontaneously or may require bone grafting.
There have been a substantial number of case reports and literature reviews published that describe the various treatment modalities for this aggressive lesion, as well as the recurrence rates associated with these modalities. There is a limited literature published with 5 years of follow-up and rehabilitation efforts into the regenerated bone. We present a case of extensive OKC involving the ramus and body of the mandible, which was treated with decompression and enucleation, followed by rehabilitation with a dental implant, and was followed up on for 6 years. We present this article in accordance with the CARE and Narrative Review reporting checklists (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-26/rc).
Case presentation
A 32-year-old female patient presented to the Department of Oral and Maxillofacial Surgery with a one-week history of pain on the left side of her lower face. The pain was associated with swelling and limited mouth opening. The medical history was noncontributory and vitals were within normal ranges. A diffuse swelling was visible on extraoral examination, extending anterio-posteriorly from the corner of the mouth to a tangent drawn along the tragus of the ear and superio-inferiorly from the ala tragus line to the inferior border of the mandible. The mouth opening was restricted to 2 cm. When palpated, the region was firm in consistency, tender to palpate, and had a local rise of temperature.
Diagnosis and treatment planning
An orthopantamogram and cone beam computed tomography (CBCT) revealed a well-defined multilocular radiolucent lesion extending from the mesial aspect of 37 into the ramus of the mandible, along with thinning of the mandibular posterior and inferior borders. Aspiration of the lesion revealed pus, indicating the possibility of an infected cyst, and it was sent for culture and sensitivity test. A comprehensive pre-surgical blood evaluation was ordered, and all parameters were within normal limits.
Decompression procedure
Given the extent of the mandible involvement, the patient’s age, and the proximity to the inferior alveolar canal, a window was created through the oral mucosa into the lumen of the cystic cavity along with extraction of 37 and an initial decompression using a section of Ryele’s tube was done (Figure 1).
The cystic lining obtained during the procedure was sent for histopathological examination (HPE). Tablets amoxycillin plus clavulonic acid combination 625 mg BIS daily and metronidazole 400 mg TID were prescribed to treat the infection. The patient and family were instructed to perform saline irrigations twice daily via tubing, with weekly check-ups. The HPE report of the incisional biopsy confirmed odontogenic keratocyst with parakeratinised epithelium. After 8 months of decompression, shrinkage in the size of the lesion was verified using CBCT, therefore was enucleated under general anesthesia, followed by the modified Carnoys’ solution application. Mucosa was primarily closed with 3-0 vicryl. The recovery from the anaesthesia was uneventful. The patient was followed up for 3 years and a series of orthopantamograms revealed spontaneous bone healing of the pathological cavity.
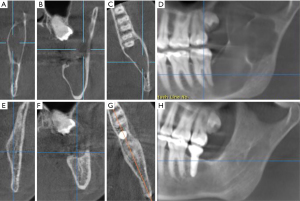
Measuring bone density for rehabilitation
A CBCT was performed at the end of 3 years to check the density of the regenerated bone (Figure 2). As the patient desired to have the missing molar replaced with a dental implant, the CBCT regions of interest (ROI) similar to grey values on the CT, were compared to calculate the mandibular cortical bone radiographic density. Three horizontal reference lines were drawn in the mandible: one along the lower border, one along the alveolar crestal bone, and one as a tangent to the sigmoid notch. The radiographic bone densities were measured between these lines, and the ROI values were compared to normal bone in the mandibular body anterior to the lesion (Figure 3). A dental implant was placed and loaded after osseointegration, based on the radiographic bone quality. After a year of follow-up, no postoperative complications related to the lesion or implant have been observed. The patient is being followed up on on a recurring basis, and there has been no evidence of recurrence in the 6 years since surgery.

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
The odontogenic keratocyst, first described by Philipsen, is an odontogenic developing cyst (1). Because of its aggressive infiltration behaviour and neoplastic nature, the World Health Organization (WHO) categorised it as a tumour in 2005 and termed it Keratocystic odontogenic tumour (KCOT). In 2017, the WHO again included under the category of cyst (3). During the second to fourth decades of life, OKC is more frequent in the posterior mandible. Because of the cyst’s medullary spread, it is frequently discovered at a later stage, after substantial bone loss has occurred (4).
Despite the fact that a wide range of treatment modalities are reported in the literature, decompression followed by enucleation with Carnoys solution has gained popularity, with resection reserved for cases of recurrence (5). Recurrence rates ranging from 0–62% have been reported in the literature with various treatment modalities (6). The most typical causes of recurrence, are reported to be insufficient cystic lining removal and the development of new primary cysts (7). It is reported that the synthesis of IL 1 and 6 by keratinocytes, elevated prostaglandin levels as factors for high recurrence rates associated with OKC (8). Multiple recurrences would lead to increased bone loss, which would increase surgical morbidity.
Initial decompression, allows the cystic lining to regresses, resulting in a reduction in total volume of the cyst and stimulating new bone formation in the walls of cystic cavity (8). Following decompression, enucleation facilitates complete removal of the cystic lining, lowering the likelihood of recurrence. This lower rate of recurrence may be related to the fact that after decompression, the recurrent parakeratinised epithelium histologically converts to non keratinised epithelium with reduced expression of Ki-67 and Bcl2 (9). Pogrel reported effective treatment of keratocysts with decompression or marsupialization followed by enucleation, with a 12% recurrence rate (10). Decompression is more successful in the mandibular body than in the ramus region, according to Nakamura et al., with the multilocular lesions and lesions in the ramus region having a higher rate of recurrence (11).
Decompression not only preserves adjacent vital structures including erupting teeth, the maxillary sinus, and the mandibular nerve, but it also maintains the bone’s anatomic integrity. After enucleation, the cystic cavity’s undamaged exterior walls can serve as a scaffold for the development of new bone. Although restoring the defect with the bone grafts has proven to stabilize the blood clot and consequently leading to accelerated bone healing, which would enable early rehabilitation in the dentate segments of jaws, their use is associated with donor site morbidity, resorption of the graft and recurrence of pathology within the graft. Chiapasco et al. studied the spontaneous bone healing after enucleation of enormous mandibular cysts in a group of 27 patients, reporting a successful resolution using a subjective and computerised study of postoperative panoramic radiographs (12).
Considering the patient’s age and the anatomic region of occurrence of pathology, the cyst was decompressed thereby regenerating new bone formation in the cystic cavity without the use of any grafts in our case.
The regenerated bone can be used to restore the patient’s functional aspect by placing osseointegrated implants. Barry and Kearns reported implant placements in the regenerated bone after bone grafting with autogenous corticocancellous iliac bone and alloplastic bone grafts (13). Table 1 depicts the various rehabilitation modalities used by surgeons, which include either immediate implant placement or delayed implants after bone formation. None of the reported case reports or series were followed up on for more than three years to see if there were any complications or failures with rehabilitation procedures (13-18).
Table 1
| Literature | Lesion and region | Treatment | Rehabilitation |
|---|---|---|---|
| Barry & Kearns, 2003 (13) | Primary OKC of mandible, Mandibular body and angle | Enucleation of lesion and immediate reconstruction with iliac bone graft | Implants after 4 months |
| Garde et al., 2010 (14) | Primary OKC of mandible (body) | Decompression followed by enucleation of lesion 4 months later and allowed for spontaneous bone healing | Rehabilitation with implants after 6 months |
| Isler et al., 2012 (15) | Primary OKC of mandible (canine to molar) | Enucleation of lesion | Immediate implant within extracted teeth sockets |
| Nilius et al., 2019 (16) | Gorlin Goltz syndrome, OKC of mandible (molar to angle) | Enucleation followed by bone graft | 6 months later rehabilitation with dental implant |
| Chacham et al., 2020 (17) | Primary OKC of mandible (body) | Enucleation and grafted with particulate bone graft | 3 months later rehabilitation with dental implants |
| Thyne et al., 1994 (18) | Recurrent OKC, mandibular body | Resection followed by primary reconstruction with Iliac bone block graft | Rehabilitation with immediate implants |
OKC, odontogenic keratocyst.
For the evaluation of regenerated bone before placing implants, in comparison to a CT and orthopantamograms, CBCT can be used as an excellent tool to measure regenerated bone density, with the advantages of minimal radiation exposure and simultaneous thorough evaluation of the lesion for any recurrence in the tomograms.
In the present case, we used a novel method to calculate bone density and compare the quality of regenerated bone to normal bone using ROI. Although CBCT grey values are considered nonspecific and cannot be interpreted as Hounsfield units (HU) of computed tomography, they could be a useful tool in treatment planning. During the follow-up period of 6 years no recurrence or implant related complications was observed.
It is possible to conclude that spontaneous bone regeneration can occur in large mandibular cysts by decompression without the use of bone grafts, thereby simplifying the surgical procedure and lowering economic and biological costs. We believe that CBCT can be used to predict bone quality, particularly when rehabilitating pathological defects, due to its low radiation exposure and cost-effectiveness. Rehabilitation using dental implants in the regenerated bone following management of pathological entities still remains challenging attributed to their recurrence rate. Therefore, long-term follow-up is needed to evaluate such lesions which requires the patient compliance.
Acknowledgments
Authors acknowledge the Department of Oral and Maxillofacial Pathology and Department of Oral and Maxillofacial Surgery, Vishnu Dental College, Bhimavaram, Andhra Pradesh, India.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE and Narrative Review reporting checklists. Available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-26/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-26/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Al-Moraissi EA, Dahan AA, Alwadeai MS, et al. What surgical treatment has the lowest recurrence rate following the management of keratocystic odontogenic tumor?: A large systematic review and meta-analysis. J Craniomaxillofac Surg 2017;45:131-44. [Crossref] [PubMed]
- Fidele NB, Yueyu Z, Zhao Y, et al. Recurrence of odontogenic keratocysts and possible prognostic factors: Review of 455 patients. Med Oral Patol Oral Cir Bucal 2019;24:e491-501. [Crossref] [PubMed]
- Speight PM, Takata T. New tumour entities in the 4th edition of the World Health Organization Classification of Head and Neck tumours: odontogenic and maxillofacial bone tumours. Virchows Arch 2018;472:331-9.
- Vijayarangan S, Baskara Pandian V. Management of the Odontogenic Keratocyst - Six Cases with Conservative Management Supported by Chemical and Electrochemical Cauterization. Cureus 2019;11:e6260. [Crossref] [PubMed]
- Pogrel MA. Decompression and marsupialization as a treatment for the odontogenic keratocyst. Oral Maxillofac Surg Clin North Am 2003;15:415-27. [Crossref] [PubMed]
- Kshirsagar RA, Bhende RC, Raut PH, et al. Odontogenic Keratocyst: Developing a Protocol for Surgical Intervention. Ann Maxillofac Surg 2019;9:152-7. [Crossref] [PubMed]
- Vallejo-Rosero KA, Camolesi GV, de Sá PLD, et al. Conservative management of odontogenic keratocyst with long-term 5-year follow-up: Case report and literature review. Int J Surg Case Rep 2020;66:8-15. [Crossref] [PubMed]
- Sigua-Rodriguez EA, Goulart DR, Sverzut A, et al. Is Surgical Treatment Based on a 1-Step or 2-Step Protocol Effective in Managing the Odontogenic Keratocyst? J Oral Maxillofac Surg 2019;77:1210.e1-7. [Crossref] [PubMed]
- Zhong WQ, Chen G, Zhang W, et al. Epithelial-mesenchymal transition in keratocystic odontogenic tumor: possible role in locally aggressive behavior. Biomed Res Int 2015;2015:168089. [Crossref] [PubMed]
- Pogrel MA. Treatment of keratocysts: the case for decompression and marsupialization. J Oral Maxillofac Surg 2005;63:1667-73. Erratum in: J Oral Maxillofac Surg 2007;65:362-3. [Crossref] [PubMed]
- Nakamura N, Mitsuyasu T, Mitsuyasu Y, et al. Marsupialization for odontogenic keratocysts: long-term follow-up analysis of the effects and changes in growth characteristics. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:543-53. [Crossref] [PubMed]
- Chiapasco M, Rossi A, Motta JJ, et al. Spontaneous bone regeneration after enucleation of large mandibular cysts: a radiographic computed analysis of 27 consecutive cases. J Oral Maxillofac Surg 2000;58:942-8; discussion 949. [Crossref] [PubMed]
- Barry CP, Kearns GJ. Case report--odontogenic keratocysts: enucleation, bone grafting and implant placement: an early return to function. J Ir Dent Assoc 2003;49:83-8. [PubMed]
- Garde JB, Kulkarni AU, Dadhe DP. Implant-based rehabilitation of a large mandibular odontogenic keratocyst with 7-year follow-up. J Int Clin Dent Res Organ 2010;2:95-7. [Crossref]
- Isler SC, Demircan S, Can T, et al. Immediate implants after enucleation of an odontogenic keratocyst: an early return to function. J Oral Implantol 2012;38:485-8. [Crossref] [PubMed]
- Nilius M, Kohlhase J, Lorenzen J, et al. Multidisciplinary oral rehabilitation of an adolescent suffering from juvenile Gorlin-Goltz syndrome - a case report. Head Face Med 2019;15:5. [Crossref] [PubMed]
- Chacham M, Almoznino G, Zlotogorski-Hurvitz A, et al. Expression of stem cell markers in stroma of odontogenic cysts and tumors. J Oral Pathol Med 2020;49:1068-77. [Crossref] [PubMed]
- Thyne GM, Hunter KM. Primary reconstruction of the mandible with iliac bone and titanium implants following resection of a recurrent odontogenic keratocyst. N Z Dent J 1994;90:56-9. [PubMed]
Cite this article as: Moturi K, Divya P, Uddarraju SR, Satyasai R, Kaila V, Budumuru A. Rehabilitation with implants succeeding conservative management of odontogenic keratocyst: a case report with a 6-year follow-up and literature review. Front Oral Maxillofac Med 2024;6:19.


