
A scoping review of utilisation of the EQ-5D questionnaire to evaluate health-related quality of life following a diagnosis of head and neck cancer
Introduction
Approximately 12,200 patients are diagnosed with head and neck cancer (HNC) in the United Kingdom annually (1). The survival rate of HNC has increased and is currently reported to be 50–60% (1). Treatment of HNC is associated with significant morbidity (2), particularly due to the critical functional and social roles of the face and surrounding structures. The implications of HNC on health-related quality of life (HRQOL) are widely recognised (2,3). As survivorship is increasing, patients are living longer with the impacts of HNC and its treatment, and so a significant emphasis on HRQOL in HNC research in recent years has emerged (2-5).
HRQOL is a multidimensional concept that broadly evaluates positive and negative aspects of a patient’s life. It incorporates not only physical and emotional facets, but includes key domains such as cultural, spiritual and financial well-being (5). It is an important outcome set following diagnosis and treatment of HNC. Indeed, from a patient perspective, HRQOL may be a more important factor in treatment decision-making than survival (3,6).
A variety of patient-reported outcome (PRO) tools have been utilised to determine the effect of treatments on patients’ HRQOL and guide clinicians regarding the future management and provision of services. The National Health Service (NHS) published a Long Term Plan for Cancer in 2019 (7), which aims to support the development of a world-leading cancer service. An important factor in this planning is a Nationally recognised Cancer Quality of Life Metric (QOL Metric) (8). After extensive pilot work, in December 2020 this QOL Metric was deployed in breast, prostate and colorectal cancer patients in England. From July 2021, this QOL Metric has been used to evaluate other cancers, including a 10% sample of HNC. As the QOL Metric applies to all cancers, two well-established HRQOL instruments are being used; a cancer-specific EORTC quality of life questionnaire (EORTC-QLQ-C30) and a non-disease-specific quality of life questionnaire: EuroQol 5 Dimensions (EQ-5D). The focus of this review is how the EQ-5D has been used and how these data are reported in the HNC literature.
The EQ-5D is a validated HRQOL tool which was first developed between 1987 and 1990. The EQ-5D covers five dimensions of QOL; mobility, self-care, usual activities, pain/discomfort and anxiety/depression, and is available in over 200 languages. There are three versions of EQ-5D including EQ-5D-3L and EQ-5D-Y (both with three levels of QOL severity) and EQ-5D-5L (with five levels of QOL severity). An EQ-5D visual analogue scale (VAS) is also a key component, which allows patients to express a quantitative measure of their overall self-perceived health status.
The scores selected for each domain in both the EQ-5D 3L and 5L questionnaires can be converted to numerical values by first coding answers between 1 and 5 for each domain. The corresponding codes (e.g., 11111) can produce up to 243 unique health state vectors for the EQ-5D 3L questionnaire and 3,125 unique vectors for the EQ-5D 5L questionnaire. Procedures for calculating health utility values and reference population values for 28 countries are available through the EuroQol website. This methodology is critical for calculation of economic outcomes such as Quality Adjusted Life Years (QALYs).
The aim of this review is to explore how researchers are utilising EQ-5D including what data is reported, serial measurements over time, comparison to reference populations and calculation of health utility values and derivative health economic outcomes. Finally, studies comparing HRQOL outcomes from this questionnaire with other established HRQOL questionnaires (in particular, EORTC-QLQ-C30) will be assessed. This review will help frame the findings of the national QoL Metric in HNC and allow for the opportunity to reflect on how the data could best be utilised to inform HNC research and patient care. This review does not examine specific HRQOL findings in detail, as these are well-reported within the literature (9). We present this article in accordance with the PRISMA-ScR reporting checklist (available at https://fomm.amegroups.com/article/view/10.21037/fomm-21-91/rc) (10).
Methods
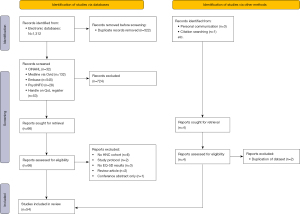
An electronic search was undertaken on the electronic databases (last updated 27/12/21): Medline via Ovid, Embase, PsycINFO and CINAHL, using a combination of MESH terms and keywords. For full details of the search strategy, see Appendix. Additionally, the HANDLE-on-QOL database was searched for studies under the categories “EQ-5D” and “Euroqol EQ-5D”. After initial deduplication of search results, title and abstract screening was undertaken in duplicate, with any uncertainty resolved by discussion among the full author team. The full texts for remaining papers, including supplementary information and appendices, where applicable, were then examined by two authors independently to determine the final list of included studies. Subsequently, two authors (EW and LT) independently undertook data extraction using a preformulated data extraction form. Any conflicts were discussed with a third author (JT) who arbitrated. Where data were incompletely reported or clarity was needed regarding a study, the corresponding author was contacted.
Studies were included if they evaluated HRQOL, self-perceived health status (by VAS) or calculated health utility values using any form of the EQ-5D questionnaire in HNC patients, or if a subgroup of HNC patients was clearly identified and reported within the study. Study designs eligible for inclusion were: randomised clinical trials, quasi-experimental studies, cohort, case-control, other longitudinal studies, cross-sectional studies or economic evaluations. Case series and case reports, as well as all review articles were excluded. We also excluded studies if they included a HNC subgroup but did not report HRQOL results for this group individually. Only papers published in English language were included.
Results
A total of 54 unique studies were included. We identified no studies published in languages other than English. There were 3 studies for which more than one report was found (5,11-15). In these instances, EQ-5D data were extracted from the study with the most readily available information, or the first published report where identical data was available. Of the 54 included studies, 20 were identified both on the Handle-on-QOL database and through other electronic searches, 24 were identified through electronic database searching only, and 7 were identified on the Handle-on-QOL database only. A further study was identified from reference list searching, and 2 more through personal communication with known experts in the field. A summary of search results, screening and selection of studies is outlined in Figure 1.
Nine studies were randomised controlled trials, of which 5 compared different chemotherapy regimens. Eight studies employed a cohort design, with 1 further study using a case-control design. There were 7 longitudinal (uncontrolled) observational studies, and 3 economic evaluations. The most frequently employed study design was cross-sectional (26 studies). The most common countries for studies were: USA (n=11), UK (n=6), The Netherlands (n=6) and Canada (n=5). In addition, 8 studies were multinational. There was 1 study from Africa, based in Egypt, and no studies from the South American continent.
Sample sizes ranged from 25 to 54,492 in the included studies and were dependent on study design and the specific population included. The mean sample size across all studies was 1,321 (SD =7,674), while the median sample size was 172 (IQR, 84–329); indicating that most studies had a relatively small sample size, with some notable outliers. The characteristics of included studies are summarised in Table 1.
Table 1
| Author and year of publication | Study design | Participants and setting | Key study outcomes and effect size (95% CI: unless otherwise specified) | EQ-5D questionnaire used and related factors | Key HRQOL findings |
|---|---|---|---|---|---|
| Interventional studies | |||||
| Del Barco Morillo, 2016 (16) | Phase 2 non-randomised, open label, controlled trial | 40 patients with confirmed metastatic and/or recurrent SCCHNC deemed untreatable by surgery or radiotherapy. 12 centres across Spain. Recruited between March 2011 to May 2012 | Panitumumab and paclitaxel combination treatment showed a disease control rate of 75%. HRQOL was preserved and there was a favourable safety profile. Progression-free survival was 7.5 months (95% CI: 4.9–8.3). Median overall survival 9.9 months (95% CI: 8.0–16.3) | EQ-5D-3L index score and VAS performed at baseline and every 8 weeks—not reported in full | EQ-5D VAS self-perceived health scores remained stable at all follow up visits (median baseline score 60, subsequent median scores ranged from 57–67). EQ-5D index also stable (median 0.7 at baseline, ranged from 0.6–0.8 at follow ups) |
| Harrington, 2017 (12); Cocks, 2019 (11) | Non-blinded two arm parallel group randomized controlled trial | 361 patients diagnosed with HNC recurrent or metastatic squamous cell carcinoma who progressed within 6 months of platinum-based chemotherapy. 66 sites within 15 countries. Recruited between May 2014 to July 2015 | Nivolumab delayed the time to deterioration of HRQOL outcomes compared to single-agent therapy. Nivolumab stabilised symptoms and functioning compared to the control group | EQ-5D-3L at baseline, week 9 and then every 6 weeks during treatment. Post treatment questionnaires at 35 and 80 days. EORTC-QLQ-C30 and EORTC-QLQ-H&N35 were also completed at the same time intervals | No clear trends in EQ-5D data for either group. Significantly larger drop in EORTC-QLQ C30 scores for control group vs. Nivolumab (≥10 points) in 8/15 domains. Similar findings for EORTC-QLQ H&N35. EQ-5D VAS significantly better in nivolumab arm |
| Harrington, 2021 (17) | Two arm parallel group randomized controlled trial | 469 patients diagnosed with recurrence or metastatic HNC squamous cell carcinoma. 97 centers across 20 countries. Recruited between December 2014 to May 2016 | HRQOL was stable in patients given pembrolizumab but declined within the control group after week 15 of treatment. Function and symptoms remained similar. Median Time to deterioration in global health scores 4.8 months for intervention, 2.8 months for control (HR 0.79, 95% CI: 0.59 to 1.05) at week 15, QoL scores stable for pembrolizumab (LSM 0.39, 95% CI: −3 to 3.78), worse for control (LSM −5.86, 95% CI: −9.68 to −2.04), LSM difference 6.25 points (95% CI: 1.32 to 11.18) | EQ-5D-3L at baseline, week 3, 6 and 9, and every 6 weeks after up to 1 year (51 weeks total), and at 30 days post treatment. ED-5D-3L not fully reported within the article. EORTC QLQ-C30 and EORTC QLQ-H&N35 questionnaires were also completed at the same time periods and reported | HRQOL was stable in patients given pembrolizumab but declined within the control group after week 15 of treatment. Function and symptoms remained similar. Median time to deterioration in global health scores 4.8 months for intervention, 2.8 months for control (HR 0.79, 95% CI: 0.59 to 1.05) at week 15, QoL scores stable for pembrolizumab but worsened for control—least-squared mean difference 6.25 points (95% CI: 1.32 to 11.18) |
| Jansen, 2021 (18) | Unblinded randomised controlled trial | 92 patients within 5 years of total laryngectomy surgery. Five HNC centers, The Netherlands. Recruited between June 2015 to January 2018 | In Tune without Cords (a self-help exercise programme) may be an effective manner of maintaining HRQOL, however is more costly than not-utilising a self-help exercise programme | EQ-5D-3L measured at baseline, 3 and 6 months follow up. EORTC QLU-C10D and SWAL-QOL were measured at the same time periods | Mean total costs €1,719 (SD 3,011) for control vs. €1,089 (SD 1,622) for intervention (P=0.22). MD −€685 for intervention, +0.06 QALYs (P<0.05). EQ5D utility values at baseline 0.76 (SD 0.26) in control vs. 0.85 (SD 0.17) in intervention. Assuming €20,000/QALY, adjusted probability of intervention being cost effective =57–64% |
| Jones, 2020 (19) | Phase 3 open-label randomised controlled trial | 334 patients diagnosed with HPV-positive oropharyngeal SCC. 32 centers internationally (1 in Ireland, 1 in The Netherlands and 30 within the UK). Recruited between November 2012 to October 2016 | Primary outcomes: 2-year survival 97.5% for cisplatin vs. 90% for cetuximab (HR 3.268, 95% CI: 1.451–7.359); 2-year recurrence rate 6.4% vs. 16% (HR 2.6, 95% CI: 1.38–5.15). Cisplatin chemoradiotherapy provided more QALYs and less costly than cetuximab bio-radiotherapy | EQ-5D-5L at baseline, end of treatment, 3, 6, 12 and 24 months post treatment. Secondary analysis of De-ESCALaTE HPV trial HRQOL data. EQ-5D-5L utility index scores reported only, no further details | No significant difference for EQ-5D utility value between intervention and control arms. Utility values decreased at end of treatment then recovered to at least BL values by 12 months follow-up |
| Mehanna, 2016 (20) | Unblinded randomised controlled trial | 564 HNC SCC patients aged over 18 years with stage 2–3 nodal disease who were eligible for chemoradiotherapy and selective neck dissection. 43 hospitals (37 centres) across the UK. Recruited between 2007 and 2012 | PET CT surveillance resulted in fewer neck dissections and saves money. Surgical complication rates were comparable between the two groups | EQ-5D (type unknown) at baseline, 2 weeks, 6 months, 12 months and 24 months. EQ-5D used to calculate QALY. Domains and VAS not reported. EORTC-QLQ-C30 and EORTC-QLQ-H&N35 data not reported | QALY is increased at 6 months for patients undergoing PET CT surveillance compared to selective neck dissection. This increase became insignificant at 24 months. Over a 2-year period PET CT surveillance was more cost efficient than selective neck dissection. Over total duration of trial, PET CT surveillance saved £1,492 per person |
| Rogers, 2020 (5); Rogers, 2021 (13) | Cluster preference randomised controlled trial | 288 patients attending Multidisciplinary Team meetings following head and neck cancer diagnosis. Two centres: Leeds Teaching Hospitals NHS Trust and Aintree NHS Hospital, UK. Recruitment between April 2017 and October 2019 | The use of the PCI increased consultation times by a mean of 1 minute (95% CI: from mean was −0.7 to +2.2 min). QoL was significantly improved in the PCI group | EQ-5D-5L at baseline. EQ-5D-5L TTO crosswalk values and VAS, all fully reported. UW-QOL v4 questionnaire and the Distress Thermometer used and fully reported | 31% of patients had overall HRQOL that was less than good, whereas 69% had HRQOL that was good or better. The UWQOL revealed salivation, pain, fear of recurrence and taste to be the most dysfunctional items in relation to HRQOL |
| Sayed, 2019 (21) | Randomised controlled trial | 60 HNC SCC patients aged over 18 years eligible for radiotherapy with blood results within certain ranges and not taking anticoagulants or had recent cerebral or retinal haemorrhages. 1 hospital in Egypt. Recruited between May 2015 and March 2018 | Intervention reduced incidence of severe (Gr 3/4) dysphagia/OM from 36.7% in control group to 3.3% in intervention group [dysphagia OR 16.22 (95% CI: 1.8–143.6), OM OR 18/86 (2.05–173.73)]. Median onsets of dysphagia 3 weeks/4 weeks in intervention/control groups. Median onsets of oral mucositis 5.5/6 weeks in intervention/control groups. Side-effect-related hospital admission reduced from 30% to 6.7% Median (IQR) duration of dysphagia 1.5 weeks (0–3.25) in intervention group; 5.5 (0–10) in control group. Median (IQR) duration of OM 0 w (0–2) in intervention group, 5 weeks (0–8.25) in control group. No impact on locoregional control | EQ-5D-3L at baseline and 3 months. EQ-5D-3L VAS and utility index reported only | EQ5D index & VAS scores were significantly reduced at 90 days follow up in the intervention group compared with control group |
| Truong, 2017 (22) | Phase 3 randomised control trial | 818 HNC SCC patients with stage 3 or 4 disease pre-treatment. Unknown hospitals in USA. Time period not specified | No statistical difference in QOL or performance status between radiotherapy/cisplatin with or without cetuximab. HPV positive cancer patients have a higher QOL and performance status than HPV negative cancer patients | EQ-5D-3L at baseline, 2 weeks from end of treatment, 3 months, year 1, 2, 3, 4 and 5. EQ-5D-3L utility index not reported for all points in time, domains unreported, VAS not used. FACT G and FACT HN summary reported | Cisplatin improved HQRoL vs. cisplatin & cetuximab at 1 year by FACT-G (3.5% between arm change, +2.88 vs. −0.93, P<0.001); largest difference in functional subscale. No difference for EQ5D index score, but usual activities worse for cetuximab group at 1 year (P=0.016) |
| Cohort studies | |||||
| Amit, 2019 (23) | Prospective cohort | 72 patients diagnosed with oropharyngeal squamous cell carcinoma. MDACC, TX, USA. Recruited between 2014–2016 | HRQOL and symptom burden improves over time regardless of treatment modality (primary surgery or non-surgical), although acute symptom profiles differ. MDASI scores improved significantly for patients at 6 months if they were treated with single modality surgery rather than radiation (P=0.04). For patients receiving multiple modalities of treatment, MDASI scores were significantly better for the surgical group at treatment completion and 6 weeks, compared to the non-surgical group. However, these differences were not present by 6 months post treatment | EQ-5D utility and VAS at baseline and 3–6 months after treatment. EQ-5D information provided in supplementary table and fully reported. MDASI scores fully reported | HRQOL and symptom burden improves over time regardless of treatment modality (primary surgery or non-surgical), although acute symptom profiles differ |
| Aoki, 2022 (24) | Prospective cohort | 100 patients with oral cancer treated with radical surgical intent. 1 hospital in Japan. Recruited between 1st May 2018 to 30th June 2020 | See HRQOL column | EQ-5D-5L and FACT-H&N before treatment, and at 1 and 3 months post treatment. Raw data scores were not reported within the text, however, comparative correlations between EQ-5D-5L and FACT-H&N were reported |
EQ-5D-5L scores appear to correlate with FACT-H&N scores during the perioperative period (rs=0.586, P<0.01). There was only a weak correlation between pre-treatment questionnaires (rs=0.295, P<0.05). Immediately following treatment, HRQOL scores were at their lowest. However, these improved significantly through time post-operatively (P<0.01). Anxiety and depression were worst pre-treatment, but improved greatly at 3 months post-operatively |
| Lango, 2016 (25) | Prospective cohort | 84 newly diagnosed HNSCC patients, treated with curative intent by radiotherapy +/− chemotherapy in a single USA oncology department. Recruited between Dec 2006–2013 | 50% of patients required gastrostomy insertion within 4 months of completing RT. Patient reported symptoms were the strongest predictors of gastrostomy placement, no other factors were associated with this. Greater baseline dysphagia predicted need for gastrostomy | EQ-5D 3L & VAS | EQ-5D VAS, problems with usual activities and pain were all significant predictors of need for gastrostomy placement. Composite dysphagia score via SWAL-QOL also significant predictor |
| Lango, 2014 (26) | Prospective cohort | 159 newly diagnosed HNSCC patients undergoing treatment with curative intent. 1 hospital in USA. Recruited between Dec 2006 to Dec 2012 | Dysphagia severity was associated with reduced QOL across all EQ-5D domains. Advanced tumour T stage and weight loss correlated with dysphagia severity and reduced QOL, but no other clinicopathological characteristics. Dysphagia independently predicted all-cause and disease-specific mortality, and disease recurrence | EQ-5D-3L and VAS at single point in time, pre-treatment. Scores for all domains and VAS reported in full for overall study sample, but not by cohort according to dysphagia status | Problems performing usual activities, pain and discomfort, depression and anxiety and VAS scores all associated with decreased survival by univariate analysis. Only pain/discomfort and VAS significant predictors for all-cause mortality in multivariate analysis |
| Marcellusi, 2015 (27) | Retrospective cohort | 79 HPV positive HNC patients and 20 control patients aged between 18–75 treated within the last 18 to 20 months. 465 patients with HPV related cancer groups studied with 135 control patients. Control group matched via characteristics. 6 research centres across Italy. Recruited between October 2008 and July 2012 | See HRQOL column. Risk factors associated with high risk of acquiring HPV were: >5 partners (P=0.004), sexually active before 18 years (P=0.034) and smoking (P=0.034). Higher levels of education were found to be protective (P<0.001) | EQ-5D-3L completed at a single point in time. Utility index reported by cancer site and for control group. Domains and VAS not reported | For anal and HNC cancer, age and QOL had statistically lower health utilities. The value of utilities lost was higher in women than men |
| Pottel, 2015 (28) | Prospective cohort | 81 HNC patients aged over 65 years undergoing curative intent radiotherapy with or without chemotherapy. 2 Hospitals in Belgium. Recruited between January 2010 and April 2012 | Fit patients defined by G-8 had higher QOL scores compared to vulnerable patients and retained their QOL more during and after treatment. 68% vulnerable at baseline, 92% at week 4 post-treatment by G8 (≤14 cut off score). Median (IQR) survival 1,095 (1,018–1,095) days for fit, 687 (338–1,095) for vulnerable. Quality adjusted survival (life months in perfect health): Fit 23.3 (18.3–27.4), vulnerable 8.8 (2.8–15.0) | EQ-5D-3L at baseline, 1 and 2 months. EQ-5D-3L utility index only reported | Fit patients regained baseline EQ-5D utility values by end of treatment, while vulnerable patients had significantly lower EQ-5D utility values before, during & after treatment G8 score was significantly correlated with EQ-5D utility values |
| van Hinte, 2021 (29) | Prospective cohort | 69 patients with cT1-2N0 oral cavity squamous cell carcinoma treated with END or SLNB. 1 hospital in The Netherlands. Recruited between January 2014 and June 2020 | Ipsilateral shoulder abduction (P=0.031) and forward flexion (P=0.039) were significantly better for the SLNB group at 6 weeks post-operatively when compared to the END and SLNB + neck dissection group | EQ-5D and EORTC-QLQ-HN35 recorded before surgery, 6 weeks, 6 months and 12 months after surgery. HRQOL data not fully reported within the manuscript | There were no significant HRQOL differences between those patients receiving END or SLNB at any point of time in their surgical journey |
| Zhang, 2018 (30) | Retrospective cohort | 74 Marijuana and 74 control patients with HNC aged over 17 years and undergoing treatment with curative intent. 1 hospital in Canada. Recruited between January 2011 and January 2015 | See HRQOL column | EQ-5D-3L at single point in time. EQ-5D-3L and ESAS summary reported | Marijuana users had significantly less pain/discomfort (mean difference 0.29, 95% CI: 0.04–1.54) and anxiety/depression (mean difference 0.74, 95% CI: 0.56–0.93) compared to the control group. They also had more appetite, were less tired, less drowsy and had a better general wellbeing |
| Case control studies | |||||
| Rogers, 2006 (6) | Case control | 224 HNC patients disease-free in 2004 compared to national reference data. 1 UK hospital. Recruited between 1992 and 2003 | HNC patients under 60 years had worse QOL compared to national reference population | EQ-5D-3L completed at a single point in time. EQ-5D-3L fully reported. UWQOL reported as correlation to EQ-5D-3L | More problems were reported with self-care/usual activities vs. the UK reference population regardless of age. In patients under 60 y there was also more pain/discomfort, anxiety/depression & less mobility reported. There was an overall prevalence of any problem in 70% of HNC cohort vs. 35% in the UK reference population for under 60s. For patients over 60 this disparity was not seen. Utility value was not related to age, nor was VAS scores for HNC cohort. There was good correlation between EQ-5D VAS and UWQOL global health rating |
| Uncontrolled longitudinal studies | |||||
| ACTION study group, 2017 (31) | Prospective longitudinal | 5,249 cancer survivors (571 mouths & pharynx), 12 months post-treatment, in 8 low-middle income countries in Southeast Asia. Recruitment period not specified | Mouth and pharynx cancers 3rd most common. See QOL column | EQ-5D-3L and Index values at a single point in time, 12 months after diagnosis | Lung cancers had lowest global QoL scores by EORTC QLQ-C30 and highest proportion of problems on EQ-5D. Clinically meaningful differences in HRQoL for >65 years old vs. younger patients across multiple domains, alongside measures of deprivation, cancer stage and co-morbidity burden |
| Aoki, 2019 (32) | Prospective longitudinal | 84 patients with oral malignancies undergoing radical treatment. Tokai University Hospital, Japan. Recruited between April 2016 to December 2017 | EQ-5D-3L and EQ-5D VAS were strongly correlated with FACT H&N scores | EQ-5D-3L and EQ-5D VAS before treatment, at completion of treatment, 1 and 3 months post treatment. EQ-5D-3L not fully reported numerically. FACT H&N data collected and correlations with EQ-5D data made | Moderate correlation of EQ-VAS and EQ-5D-3L (R2 0.467); strong correlation of EQ-5D-3L with FACT (R2 0.621); strong correlation of EQ VAS with FACT (R2 0.638). Mod correlations for ‘high risk group’, stronger for ‘low risk group’ (+ve nodes etc.). Poor correlation of EQ5D3L with EQVAS in high risk group. Correlations between EQ5D3L subscales and FACT except for SWB. Significant changes over time for FACT H&N and EQ5D3L (P=0.013, P<0.01) but not EQVAS. Lowest at treatment completion, improved over time 25% patients had max score on EQ-5D 3L |
| Beck, 2019 (33) | Prospective longitudinal | 236 patients with primary HNC treated with curative intent. Data collected for the DHNA. Netherlands Cancer Institute and Radboud University Medical Center, The Netherlands. Recruited between Nov 2014 to February 2017 | See HRQOL column | EQ-5D-3L at baseline then 3/6/12/24 months following via online survey. EQ-5D-3L utility score reported, further details not included within article. EORTC QLQ-C30 and EORTC QLQ-H&N35 completed and reported. Multiple regression models shown within paper to predict HRQOL of HNC patients | 123 (52% of participants) utility values =1. Generic domains of C30 (global health, physical, role, emotional functioning and pain) correlated well with EQ-5D utility values, cancer specific ones did not |
| Maximiano, 2018 (34) | Prospective longitudinal | 315 HNC patients aged over 18 years with moderate to severe pain. 1,711 lung, colorectal, HNC and breast patients recruited. 150 Oncology units across Spain. Recruited between June 2011 and July 2012 | See HRQOL column | EQ-5D-3L completed at baseline and 3 months. Data reported in full | Pain and QoL improved from baseline to 3 months with usual pain management for all cancer groups (P<0.001). EQ-5D index at baseline for HNC patients impacted ultimate EQ-5D scores. Presence of anxiety/depression at baseline significantly reduced improvements |
| Plaschke, 2017 (35) | Prospective longitudinal | 43 recurrent or metastatic HNC patients aged over 18 years with life expectancy greater than 3 months who have no further standard treatments available and are to be administered bleomycin and electrochemotherapy. 1 Centre from Netherlands, Spain, England, Denmark, Slovenia and Italy. Recruited between November 2011 and October 2015 | Complete response seen in 8 patients and partial response seen in 16 patients. Tumour size only character that had statistically significant effect on tumour response. No patients required acute tracheostomy after treatment. Side effects included ulceration, hyperpigmentation, suppuration, nausea, odour, dysphagia, flu, swelling, sensitivity, local defect. At 12 months, survival was 54% (CI: 31–77%) | EQ-5D (type unknown) at baseline, 1, 2, 4, 8 and 12 months. EQ-5D VAS and utility score reported in supplements for 4 of 6 countries at 0, 4 and 8 weeks. EORTC-QLQ-C30 and EORTC-QLQ-H&N35 reported in supplements | Electrochemotherapy was well tolerated by participants. Mean EQ-5D scores improved non-significantly at 2 and 4 months compared to baseline (0.67, SD 0.04 at baseline; 0.67, SD 0.05 at 4 weeks; 0.74, SD 0.05 at 8 weeks; P=0.51). |
| Sprave, 2020 (36) | Retrospective longitudinal | 49 HNC patients receiving radiotherapy. 1 Hospital in Germany. Recruited between July 2019 and November 2019 | Acute toxicities (CTCAE grade ≥3) of high frequency: dermatitis [15]; dysphagia [10]; OM [21]. Chronic toxicities (CTCAE grade ≥3) of high frequency: Xerostomia [8] | EQ-5D-5L completed pre and post radiotherapy, 3 and 6 months. EQ-5D-5L fully reported for each time interval | No significant changes in EQ-5D index values in primary/adjuvant RT subgroups were seen over time. Significant changes were seen for EQ-5D VAS in the re-irradiation subgroup. Lower index values were seen for females vs. males |
| Tsai 2021 (37) | Prospective longitudinal | 2,507 locally advanced (stage III or IV) oral SCC patients treated with curative intent (194 patients with QOL data). 1 Hospital in Taiwan. Recruited between January 2007 and December 2017 | 5 y overall survival rate 54.2%. Mean (SD) survival: 59.1 (0.8) months. Life expectancy: 8.7 (6.3–14.8) years (vs. 27.7 years for reference population). Quality-adjusted life expectancy [7.7 (6.3–14.8) years (vs. 27.7 years for reference population)] | EQ-5D-3L (Taiwanese version) within 1, 1–3 and >3 years after treatment. Utility values presented graphically only, QALYs calculated from EQ-5D but no other data recorded | Loss of 20 QALYs in oral SCC population after curative treatment compared to reference population. Swallow (8.3 years) and social eating (7.5 years) were most persistent problems reported |
| Cross-sectional studies | |||||
| Baxi, 2016 (38) | Cross sectional | 102 patients diagnosed with HPV-positive oropharyngeal cancer at least 12 months prior to recruitment, working full time at diagnosis. Memorial Sloan Kettering Cancer Center, New York, USA. Recruited between 2010–2014 | Chemotherapy and radiation treatment disrupts the working pattern of patients, however most ultimately return to work. Treatment related toxicities may lead to dissatisfaction with their ability to work | EQ-5D-3L and EQ-5D VAS at a single point in time, at least 12 months following diagnosis. EQ-5D-3L data fully reported within text. EORTC QLQ-H&N35 questionnaire also collected, no comparison between this and EQ-5D-3L scores | 55% of patients had no issues in EQ-5D, 85% of patients were able to keep working. Dissatisfaction with work was associated with more problems on EQ-5D and reduced VAS |
| Baxi, 2018 (39) | Cross sectional | 185 patients with HPV-positive oropharyngeal squamous cell carcinoma, at least 12 months following radiation. Large urban cancer centre USA. Recruited between 2010–2016 | Despite HRQOL being similar, older survivors have increased mobility and social eating issues than younger survivors | EQ-5D-3L and EQ-5D VAS at a single point in time, at least 12 months following radiotherapy. EQ-5D-3L reported as mean score with standard deviation within each domain. EORTC QLQ-H&N35 questionnaire also collected. | EQ-5D/VAS scores similar for patients regardless of age. Most significant difference between ages for mobility (MD 0.18, P=0.003). EQ-5D domains worsened with increase comorbidities—aOR mobility probs 3.14 (CI: 0.93–7.64) for >65 y, 4.58 (CI: 1.13–14.97) for ever smoking, 1.45 (CI: 0.62–7.3) for increased Charlson index vs. <65 y old patients |
| Broderick, 2020 (40) | Cross sectional | 288 patients with HNC treated with curative intent. Liverpool Head and Neck Centre, Aintree, Liverpool. Recruited between April 2017 to October 2019 | Post-treatment HNC patients with too much saliva (n=45) have comparatively reduced HRQOL scores. Saliva quantity is notably associated with tumour location, stage and treatment | EQ-5D-5L TTO crosswalk and EQ-5D VAS at single point in time post-operatively. EQ-5D data not fully reported; median IQR scores given for TTO and VAS in relation to salivation. UW-QOLv4 and Distress Thermometer scores reported in relation to salivation | Normal/enough saliva consistency for 48% of patients, too little/none for 37%, too much for 16%. EQ-5D VAS decreases 10% for too little saliva and 20% for no saliva, with more problems in every EQ-5D domain with reduced saliva |
| Cardoso, 2021 (41) | Cross sectional | 892 patients diagnosed with oropharyngeal cancer, >18 years old with no evidence of recurrence/metastases or second primary. MDACC, TX, USA. Diagnosed between Jan 2000 to Jan 2016 | Trismus was self-reported in 31% of patients and trismus appears to progress over time. Increasing trismus severity negatively impacts HRQOL. Trismus is associated with disease stage, tumour site and exposure to chemotherapy. EQ-5D VAS similarly weakly correlated, 6 patients decrease for mild, 23 patients decrease for severe trismus | EQ-5D VAS distributed via Dillman’s method at single point in time post-operatively (at least 12 months). EQ-5D VAS scores reported fully in relation to trismus severity. MDASI-HN and MDADI reported | EQ-5D VAS was weakly correlated with trismus severity; there was a 6-point decrease for mild and 23-point decrease for severe trismus |
| Davies, 2020 (42) | Cross sectional | 2,065 patients diagnosed with HNC between 2011–2014, within the Head and Neck 5000 cohort study | EQ-5D-5L and EORTC-QLQ-C30 HRQOL data was comparable, article suggested EQ-5D-5L be used preferentially in future studies | EQ-5D-5L and EQ-5D VAS at single point in time. EQ-5D-5L scores compared to EORTC-QLQ-C30 questionnaire scores and reported within article | Moderate association between QOL (by EQ-5D score) and self-perceived health (by VAS). Moderate-strong correlation with EORTC QLQ-C30 measures, index score better correlated than VAS score. EQ-5D VAS score correlates strongly with global health score on EORTC QLQ-C30 |
| Giuliani, 2019 (43) | Cross sectional | 130 patients diagnosed with any form of HNC, 64 of which were recruited at diagnosis. Princess Margaret Cancer Centre, Canada. Recruited between January 2013 to May 2014 | 48% of HNC survivors reduced their work capacity and 32.8% did not return to work following treatment. Lower HRQOL scores were associated with those unemployed or who had reduced their work hours | EQ-5D-5L and EQ-5D VAS given at a single point in time. EQ-5D-5L responses not fully reported. FACT-HNv4.0. MDASI-HN and CaSUN questionnaires also utilised | 52% of patients able to return to previous level of work after treatment. Return to work post-treatment associated with reduced MDASI-HN symptom interference scores (OR 1.1, 95% CI: 1.02–1.19). Other health utility/QoL scores were not significantly correlated with return to work |
| Jansen, 2018 (44) | Cross sectional | 288 patients who were members of the Dutch Patients’ Association of Laryngectomees, The Netherlands. Recruited in November 2014 | 54% visited GP in past 3 months, 55% visited specialist in academic centre, 42% visited specialist in general practice, total healthcare costs for highest PAM level €1,346 (SD 2,597) vs. lowest €2,282 (SD 3,798). Total societal costs for highest PAM level €1,909 (SD 3,855) vs. lowest €2,627 (SD 4,147). Differences in costs NS after adjusting for confounders & EQ-5D. Patients with better activation reported less costs, even after adjustment for confounding factors | EQ-5D-3L sent by regular post to patients at a single point in time. EQ-5D-3L data not fully reported, mean utility score alone provided | HRQOL measured by EQ-5D utility scores mitigated difference in healthcare costs, showing that this is an important contributor to cost |
| Kamal, 2018 (45) | Cross sectional | 207 survivors of HNC who had received radiation therapy. University of Michigan, USA. Time period not specified | MDASI-HN-DM score correlated with multi-item XQ scores | EQ-5D VAS score at a single point in time via phone call. MDASI-HN-DM, XQ scores and EQ-5D VAS scores were all taken at the same time, at a median of 88 months following the end of radiotherapy treatment | MDASI-HN-DM and EQ-5D VAS had inverse relationships on bivariate analysis (Spearman’s P=−0.31, P<0.001), and XQ with EQ-5D VAS (Spearman’s P=−0.38, P<0.001). Dry mouth scores, captured by any tool, were correlated with reduced HRQOL |
| Karczewska-Lindinger, 2021 (46) | Cross sectional | 64 patients diagnosed with HNC receiving treatment with curative intent. Sahlgrenska University Hospital, Sweden. Time period not specified | HNC patients spent most of their time sedentary. Higher education level, reduced physical function and higher fatigue were associated with lower physical activity levels | EQ-5D-3L at a single point in time—only two domains collected (pain/discomfort, and anxiety/depression). EQ-5D-3L data of chosen two domains reported in full. EORTC QLQ-C30 also collected, however only five domains selected (physical function, role function, pain, fatigue and insomnia) | 57% of patients expressed moderate pain/discomfort and 59% expressed moderate anxiety/depression on the EQ-5D domains selected. Physical function was highest reported domain from EORTC-QLQ-C30 with a mean of 88.7 (SD 17.5) |
| Khadela, 2021 (47) | Cross sectional | 104 patients diagnosed with newly diagnosed HNC prescribed a chemotherapy regimen. Private clinic in West India. Recruited between February 2018 to February 2020 | Clinical pharmacist services aided identification and understanding of medication-related concerns for HNC patients. It improved QALYs and decreased adverse drug reactions | EQ-5D-5L prior to each chemotherapy cycle until the completion of treatment. EQ-5D-5L data not reported within study | QALYs significantly decreased in the control group (0.012 to 0.005) who did not receive clinical pharmacist services. The QALYs of those in the intervention group stayed relatively stable (0.013 to 0.014) after the completion of six chemotherapy cycles |
| Kimman, 2015 (48) | Cross sectional | 9,153 patients recruited through the Asean CosTs In ONcology (ACTION) study, of which 1,063 had HNC. 47 Hospitals across Cambodia, Indonesia, Laos, Malaysia, Myanmar, Philippines, Thailand and Vietnam. Recruited between March 2012 to Sept 2013 | HRQOL impaired significantly with living in poor economic circumstances, regardless of gender, age and level of educational attainment | EQ-5D (unable to ascertain which type) at a single point in time. EQ-5D data not fully reported, sole mean index scores provided in relation to descriptive data. EORTC-QLQ-C30 questionnaire also utilised, no comparisons made between the two HRQOL questionnaires | The mean EQ-5D index score for those with HNC was 0.67 (SD 0.18). HRQOL impaired significantly with living in poor economic circumstances (P<0.001), regardless of gender, age and level of educational attainment |
| Kularatna, 2016 (49) | Cross sectional | 151 patients with oral potentially malignant disorders or oral cancer. Six hospitals in Sri Lanka. Time period not specified | EORTC-8D and EQ-5D-3L showed significantly different utility scores and poor correlation between all functions, apart from mobility and physical functions | EQ-5D-3L and EQ-5D VAS at a single point in time. EQ-5D-3L data fully reported. EORTC-QLQ-C30 and EORTC-8D were also reported | The lowest utility score from EQ-5D-3L was −0.72, whereas it was −0.15 from EORTC-8D. EORTC QLQ-C30 showed those who had received treatment had increased QOL compared with those waiting for treatment |
| Lastrucci, 2017 (50) | Cross sectional | 25 patients who are long term survivors of nasopharyngeal carcinoma treated with convention or intensity modulated radiotherapy. San Donato Hospital, Italy. Recruited in December 2014 (treated between Jan 1990 to December 2014) | HRQOL was found to be lower in older patients, patients who were treated with older techniques, those with xerostomia and hearing loss | EQ-5D-3L completed at a single point in time. EQ-5D-3L, FACT-NP, FACT-G, XeQOLS, PSS-HN all reported in full | Patients over 50 years old had significantly better QOL (P<0.003), as did those treated with radiotherapy (PSS-HN P=0.007, and EQ-5D-3L P=0.06). PSS-HN scoring also revealed lower QoL when late state xerostomia was present (P<0.009) or hearing loss (P=0.06) |
| McDowell, 2018 (51) | Cross-sectional | 107 patients at least 4-year disease-free after curative IMRT for NPC in a Canadian oncology centre. Recruited between Jun 2015–2016 | 4 grade 4 adverse events. 47% of patients had at least 1 grade 3 adverse event. 90% of patients required prophylactic gastrostomies, all removed at a median of 115 days after RT | EQ-5D 3L and VAS at a single time at least 4 years post IMRT. Fully reported excluding VAS | QoL by FACT-H&N influenced by marital & employment status, living with others, treatment factors. Strong correlation between QoL and anxiety/depression. Significant correlations between dysphagia, xerostomia, dysarthria and aspiration (measured with MDASI-HN) and physician-reported adverse events. Strong correlations between FACT-H&N, MDASI-HN mean symptoms scores and EQ-5D mean index score |
| Noel, 2015 (52) | Cross sectional | 100 HNC patients treated 3 months to 3 years previously with no recurrence or metastasis. 1 centre in Canada. Recruited between August 2014 and October 2014 | Indirect health utility measures may be more accurate than direct health utility measures for the health status of HNC patients | EQ-5D-5L completed at a single point in time. EQ-5D-5L partially reported. HUI3, SG and TTO partially reported | EQ-5D correlated well with VAS and HUI3. SG and TTO correlate poorly. Mean EQ5-D utility scores increased with time after treatment completion |
| Noel, 2020 (15); Noel, 2021 (14) | Cross sectional | 209 HNC patients aged over 18 years who were English speaking and had capacity. 1 centre in Canada. Recruited between November 2017 and March 2018 | See HRQOL column | EQ-5D-5L completed at a single point in time. EQ-5D-5L utility index reported only. EORTC-QLQ-C30, EORTC-QLQ-H&N35 and HUI3 partially reported | OLS model for mapping EORTC onto EQ-5D had best predictive validity to enable researchers to translate EORTC to a health utility score. Disease specific domains from HNC-QOL instruments do not correlate strongly to EQ-5D or HUI3 |
| Obeso-Benítez, 2022 (53) | Cross sectional | 30 HNC survivors and 30 paired healthy subjects matches with age and gender. 1 Hospital in Spain. Recruited between February and August 2020 | HNC patients had worse performance (P<0.001) and satisfaction (P<0.001) scores (WHO-DAS 2.0 and COPM questionnaires) compared to matched control group. QLQ-30 and QLQ-H&N35 scores were also lower in the HNC group (P<0.05). EQ-5D found significant differences between the groups, with worse HRQOL scores in the HNC group (P<0.05) | EORTC QLQ-C30 questionnaire and QLQ-H&N35 questions. EQ-5D and VAS score utilised. Raw data not reported in text (both HNC patients and control group) however summary tables published | All aspects of HRQOL were worse when scored by the QLQ-C30, QLQ-H&N35 and EQ-5D groups in the HNC group when compared to the control group. The most statistically significant of these differing outcomes in the EQ-5D questionnaire were pain, anxiety/depression and VAS (P=0.001). There was good inverse correlation between WHO-DAS 2.0 functional outcomes when compared with EQ-5D VAS (r=−0.735, P<0.001) |
| Pickard, 2016 (54) | Cross sectional | 50 HNC patients with stage 3–4 cancer. 534 patients of 11 cancer types studied. Multicentre within USA. Time period not specified | See HRQOL column | EQ-5D-3L completed at a single point in time. EQ-5D-3L partially reported. FACT-G partially reported | QOL varies depending on cancer type. VAS lowest for HNC and breast cancer patients. FACT-G physical well-being scores lowest for HNC, hepatobiliary and kidney cancer patients |
| Ramaekers, 2011 (55) | Cross sectional | 396 HNC patients treated for curative intent with radiotherapy with or without surgery, chemotherapy or both. 2 hospitals in the Netherlands. Recruited between June 2009 and March 2010 | Patients with xerostomia or dysphagia have lower QOL-VAS and utility scores | EQ-5D (type unknown) completed at a single point in time. EQ-5D VAS and utility index reported | EQ-5D utility values were significantly different for pts with toxicity vs. without (P<0.0001). For no toxicity vs. ≥ grade 1 dysphagia multivariate regression showed: grade 3 xerostomia and any level of dysphagia were significant factors associated with EQ5D utility values. Other risk factors: male, oral cavity/pharynx, surgery all associated with reduced EQ5D |
| Rogers, 2021 (13) | Cross sectional | 288 HNC patients (140 in intervention PCI group). 205 HNC patients reported at 12 months. 2 UK hospitals. Recruited between January 2017 and December 2018 | Median number of items selected was 5 (IQR, 2–9), 9% selected ≥15 items. Fatigue was 6th most frequently selected item. Fatigue was more frequent in advanced tumours and pts receiving radio/chemotherapy. PCI fatigue group had significantly worse QoL scores | EQ-5D-5L at baseline and 12 months—fully reported except for VAS score. UWQOL fully reported | Fatigue was inversely correlated with HRQOL—reported in 11% of patents with very good/outstanding QOL, 55% of pts with poor/very poor overall QoL. Also correlated with EQ-5D VAS and utility values, along with all domain scores |
| Setiawan, 2018 (56) | Cross sectional | 34 nasopharyngeal cancer and 26 HNC patients aged over 18 years with HPV associated cancer and no chronic comorbidities. 116 patients with HPV cancers studied. 1 Hospital in Indonesia. Recruited between 2010 and 2015 | EQ-5D is reliable questionnaire for HPV related cancers. HNC patients had the lowest QoL scores of any cancer type | EQ-5D-5L completed at a single point in time. EQ-5D-5L domains reported. EORTC-QLQ-C30 reported as correlation to EQ-5D-5L | Excellent test-retest reliability for each EQ5D subscale (ICC >0.8). Good for VAS (ICC =0.73). Good internal consistency (Cronbach a =0.84). Generally good correlation with subdomains of EORTC QLQ-C30 and global health domain. VAS relatively high for all cancers. UV moderately high (0.69±0.1), lowest value for HNC (0.58±0.35) |
| Singh, 2021 (57) | Cross sectional | 577 HNC SCC patients aged over 18 years with recurrence or metastasis who are platinum sensitive but naive or previously treated more than 6 months previously. 195 medical/clinical oncologists from France, Germany, Italy, Spain and the UK. Recruited between January 2019 and May 2019 | FACT-G, FACT H&N, EQ-5D and VAS were lower for HNC SCC patients than referenced normal values. HNC impacts significantly on a patient’s ability to work. Caregiver QoL burden correlated to patients QOL. 5% on sick leave at diagnosis, 28% at time of enrolment. 37% in full/part time employment at diagnosis vs. 14% on enrolment. Work impairment by WPAI of 43% due to disease. 18% work time missed due to R/M HNSCC impaired work 38%. Overall activity impairment—38% | EQ-5D-3L completed at a single point in time. EQ-5D-3L group reported for all domains except mobility. FACT-G and FACT H&N partially reported | Diminished QoL was seen that was significantly lower than national reference values for FACT-G (54.1 vs. 80.9 for all cancers). Lowest scores were seen in France, highest in the UK. The same trend was seen for FACT-H&N. High level of interference with activities of daily living (44% scored 4–7) correlates with HRQOL |
| Singh, 2021 (58) | Cross sectional | 158 HNC aged over 18 years with recurrence or metastasis and post platinum 1L treatment. 82 medical/clinical oncologists from Spain and Italy. Recruited between October 2018 and February 2019 | EXTREME or cetuximab-based regimens most common (Italy 42.8%, Spain 63.1%). Whereas platinum and immunotherapy were preferred in Italy vs. Spain. Less than 1/3 of decisions conformed to national guidelines QoL scores were lower for HNC patients with recurrence or metastasis compared to other advanced cancer populations | EQ-5D-5L/3L crosswalk completed at a single point in time. EQ-5D-5L/3L crosswalk fully reported. FACT-G and FACT H&N fully reported | QoL considered for 30% of pts in Spain & 19% in Italy. EQ-5D utility values were higher in Italy vs. Spain. Spain also had more problems with usual activities, pain/discomfort, anxiety/depression. EQ-5D VAS was also significantly higher in Italy vs. Spain. All values were significantly lower than reference norm values. FACT-G scores were lower than the reference population and patients with other advanced cancers |
| Stephens, 2020 (59) | Cross sectional | 209 HNC patients aged over 18 years, English speaking with no recurrence or for palliation. 1 hospital in Canada. Recruited between November 2017 and March 2018 | UWQOL scores mapped best onto EQ-5D | EQ-5D-5L/3L crosswalk. Completed at a single point in time. EQ-5D-5L/3L utility index only reported. EORTC-QLQ-C30, EORTC-QLQ-H&N35, HUI3 and UWQOL all reported | 10 UWQOL domains could be mapped to EQ-5D. R2=0.628 for this reduced model. Global QoL question correlated strongest with HUI-3. R2=0.628 for reduced model. EQ5D was better than HUI-3—able to discriminate between several indices of disease severity by subgroup analysis |
| Thankappan, 2022 (60) | Cross sectional | 144 internal validation and 80 external validation patients with HNC aged over 18 years and at least 6 months post treatment with no signs of recurrence. Unknown hospitals across India. Time period not specified | Their developed OLS model is a reliable tool in mapping non QOL PCI onto EQ-5D utility index in order to estimate cost utility in economic evaluation studies. | EQ-5D-5L completed for internal and external at single point in time, 3 months apart -fully reported | Most patients had no/some problems for all domains. Reduced model with 5 PCI domains was the best predictor (R2=0.295). More items being selected on PCI resulted in lower HRQoL/EQ-5D utility value. For the external validation sample the R2 was 0.327 |
| Tyler, 2020 (61) | Cross sectional | 114 HNC patients aged over 18 years with sinonasal or nasopharyngeal malignancies whom completed curative treatment greater than 12 months prior with no signs of recurrence. 1 Hospital in USA. Recruited between 2001 and 2013 | Strong correlation between 3 QoL tools. There was no statistical difference between QoL for sinonasal and nasopharyngeal cancers or between treatment modalities. VAS QOL approximated to reference values for USA population | EQ-5D-5L completed at single point in time. EQ-5D-5L VAS score only used and fully reported. MDASI-HN and anterior skull base questionnaire summary reported | Negative correlation between MDASI-22 & ASBQ sum scores (Spearman’s Rho 0.74). Negative correlation between MDASI-22 & EQ5D VAS (Spearman’s Rho 0.65). Advanced Stage of tumour = worse ASBQ scores |
| Economic evaluations | |||||
| Lai, 2021 (62) | Economic evaluation | 875 patients diagnosed with non-metastatic nasopharyngeal cancer. Four Hospitals within Taiwan. Diagnosed between June 2009 to June 2013. Recruited between October 2013 to December 2017 | See HRQOL outcomes column | EQ-5D-3L at a single point in time. EORTC-QLQ-C30 and EORTC-QLQ-H&N35 also completed. EQ-5D-3L not reported | Estimated life expectancy and quality-adjusted life expectancy is 15.5 and 14.3 years respectively following NPC diagnosis. This is significantly less than the reference population (29.5 and 29.5 years) |
| Lai, 2021 (63) | Economic evaluation | 42,938 oral cancer patients and 11,554 nasopharyngeal cancer patients from the Taiwan Cancer Registry. Nationwide data collection within Taiwan. Recruited between 2011–2018 | HRQOL utility values vary between types of cancer (14 recorded within this study). Successful prevention of liver, lung, oesophagus or NPC would save >10 QALY years and $USD21,000 per case | EQ-5D at a single point in time. Specific EQ-5D questionnaire utilised is not reported. EQ-5D and WHOQOL-BREF questionnaires utilised. Scores not reported | Sex, age, stage of cancer all have significant impact on HRQOL (P<0.0001). The lifetime cost of oral cancer in males was 48.7, SD 47.3–50.1 and in females was 44.8, SD 40.1–49.6 (95% CI: ×103 USD) |
| van der Linden, 2016 (64) | Economic evaluation | 62 HNC patients with T1-2, N0 disease. 4 Centres in the Netherlands. Time period not specified | Sentinel lymph node biopsy has the biggest gain in QALYs compared to ultrasound guided fine needle aspiration cytology over a 5–10-year period. Over a lifetime, elective selective neck dissection may be preferred treatment modality. See HRQOL column | EQ-5D (type unknown) at single point in time. EQ-5D data taken from Flach et al. (9). Utility index partially reported. QALYs fully reported | Sentinel lymph node biopsy with neck dissection and/or radiotherapy in positive cases, watchful wait in negative cases resulted in the highest QALY gain over 5–10 years. However, over a lifetime, elective neck dissection resulted in the highest QALY gain |
SCC, squamous cell carcinoma; HNC, head and neck cancer; MDACC, MD Anderson Cancer Centre; HNSCC, head and neck squamous cell carcinoma; HPV, human papilloma virus; END, elective neck dissection; SLNB, sentinel lymph node biopsy; DHNA, Dutch Head and Neck Audit; IMRT, intensity-modulated radiotherapy; NPC, nasopharyngeal cancer; PCI, patient concerns inventory; 95% CI, 95% confidence interval; HRQOL, health-related quality of life; HR, hazard ratio; LSM, least squares mean; QALY, quality-adjusted life year; PET, positron emission tomography; CT, computed tomography; OM, oral mucositis; OR, odds ratio; IQR, interquartile range; MDASI, MD Anderson Symptom Inventory; RT, radiotherapy; EQ-5D, Euroqol 5 dimensions; VAS, visual analogue scale; FACT H&N, functional assessment of cancer therapy-head and neck; CTCAE, common terminology criteria for adverse events; SD, standard deviation; GP, general (medical) practitioner; PAM, plasma activated medium; MDASI-HN-DM, MD Anderson symptom inventory-head and neck-dry mouth; XQ, Xerostomia questionnaire; COPM, Canadian Occupational Performance Measure; WPAI, work productivity and activity impairment; R/M, recurrent/metastatic; UWQOL, University of Washington Quality of Life; OLS, ordinary least squares; TTO, time trade-off; MDASI-HN, MD Anderson symptom inventory-head and neck; MDADI, MD Anderson dysphagia inventory; MD, mean difference; SWB, social wellbeing; aOR, adjusted odds ratio; probs, problems; PSS-HN, performance status scale-head and neck cancer patients; SG, standard gamble; ICC, intraclass correlation coefficient.
Similarly, study populations varied considerably. Most studies included patients treated with curative intent and disease free at the time of inclusion. However, 3 chemotherapy trials specified that patients should have recurrent, metastatic disease deemed untreatable by primary surgery/radiotherapy. Of note, the worst self-perceived health status (VAS scores) was seen in Maximiano, where 27% of patients receiving chemotherapy and 14% of radiotherapy patients were palliative (34). The next lowest VAS scores were seen in Plaschke, who included patients with incurable disease (35); then Singh (57) and Singh (58), whose inclusion criteria specified patients with recurrent/metastatic disease, of stage III or IV. In all 3 studies, chemotherapy was the primary treatment of choice. The EQ-5D index values were typically lowest in studies where patients were treated by primary radio/chemotherapy [e.g., Jones—mean utility value 0.565 in Cetuximab arm (20); Singh—mean utility value 0.57 (57)]. The worst health states occurred in the immediate post-treatment period, and then recovered to baseline values or higher in the following months where repeat measures were shown [e.g., Pottel—mean utility value 0.66 at baseline, 0.42 at 1 month post-treatment, recovering to 0.66 at and 5 months. Note, subsequent drop in utility value is due to mortality over the study observation period, not reduction in QOL (21)]. A number of additional factors were identified for increased risk of reduced QOL, such as sex, age >65, tumour stage, anatomical site and comorbidities, but these were not consistent across studies. Only 4 studies specifically measured EQ-5D at least 18 months post-diagnosis for the whole sample (20-23).
At domain-level, data were reported in 13 studies for EQ-5D 3L, with 6 studies reporting the EQ-5D-5L at domain-level (Tables 2,3). In addition, 22 studies reported EQ-5D VAS scores (Table 4). Most frequently, the EQ-5D was used to calculate health utility values (23 studies, Table 5). Reporting practice varied considerably among studies. Partial domain data were reported in 2 studies, while mean scores were reported in a further 2 studies. In 3 studies, domains were grouped to form dichotomous outcomes (problems vs. no problems). Only 8 studies included the EORTC QLQ-C30 index (Figure 2).
Table 2
| Total sample size | Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No Problems | Some problems | Unable | No Problems | Some problems | Unable | No Problems | Some problems | Unable | None | Moderate | Extreme | None | Moderate | Extreme | ||||||||||
| EQ-5D 3L | ||||||||||||||||||||||||
| Kularatna, 2016 (49) | 151 | 76.2 | 22.5 | 1.3 | 86.1 | 12.6 | 1.3 | 70.9 | 27.1 | 2.0 | 41.7 | 52.3 | 6 | 60.3 | 37.1 | 2.7 | ||||||||
| Baxi 2016 (38) | 102 | 55 | 13 | 32 | 55 | 3 | 42 | 55 | 12 | 23 | 55 | 30 | 15 | 55 | 22 | 23 | ||||||||
| Karczewska-Lindinger, 2021 (46) | 64 | – | – | – | – | – | – | – | – | – | 39 | 57 | 4 | 33 | 59 | 9 | ||||||||
| Lastrucci 2017 (50) | 25 | 88 | 12 | 0 | 84 | 12 | 4 | 72 | 24 | 4 | 52 | 36 | 12 | 64 | 32 | 4 | ||||||||
| Maximiano, 2018 (34) | BL 315 | 80 | 18.7 | 1.3 | 67 | 30.1 | 2.9 | 28.9 | 61.6 | 9.5 | 2.9 | 50.8 | 46.3 | 29.8 | 55.6 | 14.6 | ||||||||
| 3-month 315 | 83.2 | 15.2 | 1.6 | 70.5 | 27.6 | 1.9 | 45.1 | 49.5 | 5.4 | 39.7 | 53.7 | 6.7 | 55.6 | 38.1 | 6.3 | |||||||||
| Pickard, 2016 (54) | 50 | 64 | 36 | 94 | 6 | 26 | 74 | 26 | 74 | 42 | 58 | |||||||||||||
| Rogers, 2006 (6) | 224 | 60 | 39 | 0.5 | 77 | 23 | 0.5 | 56 | 37 | 7 | 50 | 48 | 2 | 67 | 31 | 2 | ||||||||
| Singh, 2021 (57) | 577 | – | – | – | 59 | 41 | 36 | 62 | 22 | 78 | 29 | 71 | ||||||||||||
| Zhang, 2018 (30) | 74 | Marijuana: mean 1.22 (SD 0.41) |
Marijuana: mean 1.11 (SD 0.16) |
Marijuana: mean 1.31 (SD 0.48) |
Marijuana: mean 1.53 (SD 0.58) | Marijuana: mean 1.34 (SD 0.53) | ||||||||||||||||||
| 74 | Control: mean 1.26 (SD 0.47) |
Control: mean 1.12 (SD 0.37) |
Control: mean 1.36 (SD 0.59) |
Control: mean 1.82 (SD 0.66) | Control: mean 2.08 (SD 0.61) | |||||||||||||||||||
| Baxi, 2018 (39) | 185 | <65 years old: mean 1.078 (SD 0.269); >65 years old: mean 1.258 (SD 0.445) | <65 years old: mean 1.03 (SD 0.211); >65 years old: mean 1.00 (SD 0) | <65 years old: mean 1.143 (SD 0.387); >65 years old: mean 1.097 (SD 0.301) | <65 years old: mean 1.281 (SD 0.465); >65 years old: mean 1.200 (SD 0.407) | <65 years old: mean 1.268 (SD 0.487); >65 years old: mean 1.226 (SD 0.497) | ||||||||||||||||||
| Lango 2014 (26) | 159 | 91 | 9 | 0 | 98 | 2 | 0 | 86 | 14 | 0 | 50 | 45 | 5 | 60 | 37 | 3 | ||||||||
| ACTION study group 2017 (31)* | 571 | 82 | 18 | 86 | 14 | 77 | 23 | 51 | 49 | 53 | 47 | |||||||||||||
| McDowell 2018 (51) | 102 | 70 | 30 | 0 | 96 | 4 | 0 | 70 | 30 | 0 | 60 | 37 | 3 | 65 | 29 | 6 | ||||||||
*, estimated from figures, numerical data not available. SD, standard deviation. BL, baseline.
Table 3
| Domain | Total sample size | Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||||||
| EQ-5D 5L | ||||||||||||||||||||||||||||||
| Davies, 2020 (42) | 2,065 | 71 | 9.5 | 15.7 | 3.5 | 0.3 | 90.3 | 3.9 | 4.9 | 0.6 | 0.36 | 66.4 | 12.4 | 17.7 | 1.6 | 1.9 | 33.4 | 25.4 | 32.9 | 5.1 | 3.2 | 46.4 | 23.2 | 25.6 | 2.6 | 2.2 | ||||
| Rogers, 2021 (13) | 288 | 62.5 | 14.9 | 14.6 | 6.9 | 1 | 77.1 | 11.8 | 10.1 | 7 | 0.3 | 49.7 | 25.7 | 17.7 | 4.2 | 2.8 | 36.1 | 33.3 | 23.3 | 6.6 | 0.7 | 50.3 | 33 | 13.2 | 1.4 | 2.1 | ||||
| 205 | 65.9 | 16.6 | 12.7 | 3.4 | 1.5 | 82.9 | 9.3 | 5.3 | 2 | 0.4 | 65.0 | 20.5 | 9.4 | 4.5 | 0.5 | 46.8 | 33.7 | 14.2 | 4.9 | 0.4 | 51.7 | 30.7 | 14.6 | 2.4 | 0.4 | |||||
| Setiawan, 2018 (56) | 34 | NPC: 76.47 | NPC: 23.53 | NPC: 91.18 | NPC: 8.82 | NPC: 44.12 | NPC: 55.88 | NPC: 32.35 | NPC: 67.65 | NPC: 44.12 | NPC:55.88 | |||||||||||||||||||
| 26 | HNC: 80.77 | HNC: 19.23 | HNC: 92.31 | HNC: 7.69 | HNC: 80.77 | HNC: 19.23 | HNC: 53.85 | HNC: 46.15 | HNC: 46.15 | HNC:53.85 | ||||||||||||||||||||
| Singh, 2021 (58) | 90 | Italy: 69 | Italy: 26 | Italy: 4 | Italy: 1 | Italy: 0 | Italy: 68 | Italy: 25 | Italy: 6 | Italy: 1 | Italy: 0 | Italy: 47 | Italy: 42 | Italy: 9 | Italy: 2 | Italy: 0 | Italy: 20 | Italy: 42 | Italy: 33 | Italy: 2 | Italy: 1 | Italy: 24 | Italy: 35 | Italy: 27 | Italy: 8 | Italy: 7 | ||||
| 68 | Spain: 65 | Spain: 29 | Spain: 6 | Spain: 0 | Spain: 0 | Spain: 78 | Spain: 19 | Spain: 3 | Spain: 0 | Spain: 0 | Spain: 34 | Spain: 50 | Spain: 7 | Spain: 7 | Spain: 1 | Spain: 10 | Spain: 38 | Spain: 43 | Spain: 9 | Spain: 0 | Spain: 22 | Spain: 31 | Spain: 25 | Spain: 19 | Spain: 3 | |||||
| Sprave, 2020 (36) | BL 49 | 69.4 | 12.2 | 12.2 | 4.1 | 2 | 81.6 | 12.2 | 4.1 | 0 | 2 | 57.1 | 22.4 | 12.2 | 6.1 | 2 | 34.7 | 22.4 | 32.7 | 10.2 | 0 | 59.2 | 32.7 | 6.1 | 2 | 0 | ||||
| RT end 49 | 63.3 | 18.4 | 14.3 | 4.1 | 0 | 81.6 | 12.2 | 4.1 | 0 | 2 | 32.7 | 44.9 | 14.3 | 6.1 | 2 | 28.6 | 24.5 | 32.7 | 14.3 | 0 | 61.2 | 26.5 | 8.2 | 4.1 | 0 | |||||
| 3-mo 49 | 71.4 | 16.3 | 4.1 | 8.2 | 0 | 73.5 | 22.4 | 2 | 2 | 0 | 49 | 34.7 | 10.2 | 6.1 | 0 | 42.9 | 20.4 | 26.5 | 10.2 | 0 | 69.4 | 22.4 | 2 | 6.1 | 0 | |||||
| 6-mo 49 | 65.3 | 18.4 | 12.2 | 4.1 | 0 | 77.6 | 16.3 | 4.1 | 2 | 0 | 49 | 32.7 | 12.2 | 6.1 | 0 | 40.8 | 24.5 | 26.5 | 8.2 | 0 | 65.3 | 20.4 | 10.2 | 4.1 | 0 | |||||
| Thankappan, 2022 (60) | 144 | Int: 87.5 | 10.4 | 1.4 | 0.7 | 0 | 97.2 | 2.8 | 0 | 0 | 0 | 95.1 | 3.5 | 1.4 | 0 | 0 | 83.3 | 13.9 | 1.4 | 1.4 | 0 | 84.7 | 13.2 | 2.1 | 0 | 0 | ||||
| 80 | Ext: 86.3 | 7.5 | 6.3 | 0 | 0 | 96.3 | 2.5 | 1.3 | 0 | 0 | 90 | 5 | 5 | 0 | 0 | 72.5 | 20 | 6.3 | 1.3 | 0 | 90 | 5 | 2.5 | 1.3 | 1.3 | |||||
For functional domains: 1, no problems; 2, slight problems; 3, moderate problems; 4, severe problems; 5, unable. For symptom domains: 1, none; 2, slight; 3, moderate; 4, severe; 5, extreme. NPC, nasopharyngeal cancer; HNC, head and neck cancer; BL, baseline; RT, radiotherapy; mo, months; Int, internal (validation cohort); Ext, external (validation cohort).
Table 4
| Study, date | Number of participants | Mean (unless otherwise stated) | SD (range) |
|---|---|---|---|
| Amit, 2019 (23) | 72 | Baseline surgical: 81.36; baseline non-surgical: 82.37 | 6.08; SD 6.45 |
| 6 months post-Tx surgical: 89.9; 6 months post-Tx non-surgical: 83.9 | 4.80; 4.80 | ||
| Cardoso, 2021 (41) | 892 | 81.05 | 16.72 |
| Davies, 2020 (42) | 2,065 | Median 75 | IQR 60–90 (0–100) |
| Giuliani, 2019 (43) | 130 | Median 0.96 | IQR 0.92–0.99 |
| Baxi, 2016 (38) | 102 | 86 | 13 |
| Baxi, 2018 (39) | 185 | 85 | 14 |
| Aoki, 2019 (32) | 84 | 70 | SD 18.22 |
| Del Barco Morillo, 2016 (16) | 40 | Median 60 | NR |
| Maximiano 2018 (34) | Baseline: 315 | Baseline: 49.3; 3 months follow up: 65.7 | 18.8; 18.4 |
| Noel, 2015 (52) | 100 | 0.76 | 0.19 |
| Pickard, 2016 (54) | 50 | 61.8 | 21.7 |
| Plaschke, 2017 (35) | Baseline: 30; 4 weeks follow up: 23; 8 weeks follow up: 21 | 58.8; 55; 53.9 | 3.5; 4; 4.2 |
| Ramaekers, 2011 (55) | 396 | 75 | 15 |
| Rogers, 2006 (6) | 224 | 74 | 1 |
| Sayed, 2019 (21) | 60 | Baseline intervention: median 70; baseline control: median 70 | IQR 60–80; IQR 57.5–80 |
| 3 months post intervention: median 80; 3 months control: median 70 | IQR 70–90; IQR 50–80 | ||
| Setiawan, 2018 (56) | NPC: 34 | 75.47 | 16.99 |
| HNC: 26 | 76.03 | 15.59 | |
| Singh, 2021 (57) | 577 | 56.4 | – |
| Singh, 2021 (58) | Italy : 90 | 57.6 | 17.5 |
| Spain: 68 | 50.7 | 18.2 | |
| Sprave, 2020 (36) | 49 | Baseline: 63.88; end of radiotherapy: 63.67; 3 months follow up: 63.67; 6 months follow up: 65.2 | 20.72; 20.72; 21.81; 22.41 |
| Tyler, 2020 (61) | 114 | 74 | 21 |
| Lango, 2014 (26) | 159 | Median 85 | IQR 70–90 |
| Lango, 2016 (25) | 84 | Median 80 | IQR 70–90 |
| Obeso-Benítez, 2022 (53) | 30 | 71.62 | 20.67 |
VAS, visual analogue scale; Tx, treatment; SD, standard deviation; IQR, interquartile range; NR, not reported.
Table 5
| Study, date | Total number of participants | Time | Mean | Standard deviation | Algorithm used | |
|---|---|---|---|---|---|---|
| Davies, 2020 (42) | 2,065 | Single point | 0.87* (0.77–0.94); N<0: 10 | – | EUROQOL value set for England | |
| Beck, 2019 (33) | 236 | Single point | 0.83 | 0.18 | EUROQOL | |
| Del Barco Morillo, 2016 (16) | 40 | Baseline | 0.7* | – | Unspecified | |
| Follow ups | 0.6–0.8* | |||||
| Lai, 2021 (63) | 54,492 | Single point | Male oral: 0.9; Male NPC: 0.82 | – | Unspecified | |
| Jones, 2020 (19) | 334 | Baseline | Cisplatin: 0.836; Cetuximab: 0.812 | 0.147; 0.153 | EUROQOL | |
| Post treatment | Cisplatin: 0.606; Cetuximab: 0.565 | 0.223; 0.231 | ||||
| 3 months | Cisplatin: 0.797; Cetuximab: 0.757 | 0.145; 0.173 | ||||
| 6 months | Cisplatin: 0.827; Cetuximab: 0.784 | 0.153; 0.176 | ||||
| 12 months | Cisplatin: 0.862; Cetuximab: 0.8.25 | 0.144; 0.194 | ||||
| 24 months | Cisplatin:0.867; Cetuximab: 0.846 | 0.139; 01.44 | ||||
| Jansen, 2021 (18) | 92 | baseline | Intervention: 0.85; Control: 0.76 | 0.17; 0.26 | Dutch algorithm (not EUROQOL) | |
| 3 months | Intervention: 0.86; Control: 0.78 | 0.21; 0.25 | ||||
| 6 months | Intervention: 0.88; Control: 0.77 | 0.19; 0.26 | ||||
| Maximiano, 2018 (34) | 315 | Baseline | 0.51 | 0.1 | Spanish algorithm (not EUROQOL) | |
| 3 months | 0.72 | 0.23 | ||||
| Noel, 2020 (15) | 209 | Single point | 0.84 | 0.12 | Canada algorithm (not EUROQOL) | |
| Noel, 2021 (14) | 209 | Single point | 0.84 | 0.12 | “US population tariffs” unreferenced | |
| Noel, 2015 (52) | 100 | Single point | 0.82 | 0.18 | Algorithm reported in full in text | |
| Pickard, 2016 (54) | 50 | Single point | 0.76 | 0.15 | USA algorithm (not EUROQOL) | |
| Plaschke, 2017 (35) | 30 | Baseline | 0.67 | 0.04 | Unspecified | |
| 23 | 4 weeks | 0.67 | 0.05 | |||
| 21 | 8 weeks | 0.74 | 0.05 | |||
| Pottel, 2015 (28) | 81 | Reported for all patients (also subdivided for fit/vulnerable) | Belgium algorithm (not EUROQOL) | |||
| baseline | 0.66 (0.55–0.76)* | – | ||||
| 1 month | 0.42 (0.26–0.73)* | – | ||||
| 2 months | 0.66 (0.29–0.76)* | – | ||||
| 5 months | 0.66 (0.27–0.76)* | – | ||||
| 12 months | 0.64 (0.00–0.76)* | – | ||||
| 24 months | 0.29 (0.00–0.76)* | – | ||||
| 36 months | 0.00 (0.00–0.67)* | – | ||||
| Ramaekers, 2011 (55) | 396 | Single point | 0.85 | 0.18 | UK algorithm (not EUROQOL) | |
| Sayed, 2019 (21) | 60 | Baseline | Intervention: 0.833 (0.776–0.857)* | Zimbabwe algorithm (not EUROQOL) | ||
| Control: 0.79 (0.744–0.893)* | ||||||
| 3 months | Intervention: 0.8555 (0.79–1)* | |||||
| Control: 3 months 0.79 (0.674–0.845)* | ||||||
| Setiawan, 2018 (56) | 34 | Single point | NPC 0.75 | 0.3 | Thailand algorithm (not EUROQOL) | |
| 26 | Single point | HNC 0.58 | 0.33 | |||
| Singh, 2021 (57) | 577 | Single point | 0.57 | – | Unspecified | |
| Singh, 2021 (58) | 90 | Single point | Italy: 0.82 | – | UK algorithm (not EUROQOL) | |
| 68 | Single point | Spain: 0.69 | – | |||
| Sprave, 2020 (36) | 49 | Baseline | 0.837 | 0.17 | Unspecified | |
| Post radiotherapy | 0.828 | 0.16 | ||||
| 3 months | 0.855 | 0.15 | ||||
| 6 months | 0.856 | 0.14 | ||||
| Stephens, 2020 (59) | 209 | Single point | 0.838 | – | UK EUROQOL | |
| Thankappan, 2022 (60) | 144 | Single point | Internal: 0.911 | 0.146 | Thailand algorithm (not EUROQOL) | |
| 80 | Single point | External: 0.889 | 0.172 | |||
| Truong, 2017 (22) | 818 | 3 months | Cetuximab: 0.77; control: 0.78 | 0.15; 0.18 | USA algorithm (not EUROQOL) | |
| 1 year | Cetuximab: 0.84; control: 0.84 | 0.16; 0.17 | ||||
| McDowell, 2018 (51) | 102 | Single point | 0.85 | 0.16 | USA algorithm (not EUROQOL) | |
*, median and IQR displayed. N, number; NPC, nasopharyngeal carcinoma; HNC, head and neck cancer; IQR, interquartile range.

Studies excluded following full text appraisal are summarised in Table 6.
Table 6
| Author and year of publication | Study design | Reason for exclusion |
|---|---|---|
| Bäuerle, 2021 (65) | Cross sectional | No head and neck cancer cohort with quality of life data |
| Chan, 2014 (66) | Mathematical modelling | No EQ-5D quality of life data reported |
| Deckard, 2015 (67) | Cohort study | No head and neck cancer cohort with quality of life data |
| Gao, 2009 (68) | Cross sectional | No head and neck specific quality of life EQ-5D data reported |
| Heutte, 2014 (69) | Review article | Review article |
| Jansen, 2017 (70) | Study protocol | No head and neck cancer cohort with quality of life data |
| Protocol paper | ||
| Krebber, 2012 (71) | Study protocol | Protocol paper |
| Meregaglia and Cairns, 2017 (72) | Systematic review | Review article |
| Mozzanica, 2021 (73) | Cohort study | No EQ-5D quality of life data reported |
| Nichols, 2020 (74) | Study protocol | Protocol paper |
| Ryu, 2019 (75) | Secondary data analysis | No head and neck cancer cohort with quality of life data |
| Schwarzinger, 2019 (76) | Cross sectional | No EQ-5D given to study participants |
Discussion
With recent improvements in survival of HNC patients following treatment, HRQOL is increasingly recognised as an important metric, both for patient-centred treatment outcomes and economic utility (13). The EQ-5D is one of the most frequently employed generic QoL indices in medicine, likely due to its extensive validation in a variety of settings (including cancer) and the potential to calculate cost-utility values and QALYs. To our knowledge, this review is the first systematic examination of the use of this tool in HNC patients.
Given the versatility of the EQ-5D and multiple components/versions, it is unsurprising that its use was highly variable. However, a number of studies which specified that EQ-5D was used did not report the results of this index. We tried to contact authors for this information in these instances, or where data reporting was incomplete, but response rates were low. Several studies preferentially reported cancer-specific QOL tools such as MDASI, UW-QOL, EORTC-QLQ-C30 or EORTC-QL-H&N35 and only partially reported EQ-5D. However, these tools lack the facility to produce health index values and economic outcomes. Where multiple tools were used, EQ-5D appeared to be at least as effective at detecting global QOL and health states and discriminated between objective levels of disease severity. However, by design, the generic nature of the EQ-5D domains meant that some cancer-specific concerns and problems were not detected. It is therefore advisable to include both a cancer-specific QOL index combined with the EQ-5D to maximise the value of study data.
A number of studies only reported VAS scores or dichotomised responses into ‘problems’ and ‘no problem’ groups. While VAS gives an excellent indication of a patient’s self-perceived health status, inclusion of utility values or full domain-specific responses helps to identify discrepancies between self-perceived health status and arguably more objective functional/symptom burden. Similarly, a number of studies recorded full 5-domain data but then dichotomised this into ‘problems’ and ‘no problems’. This can be useful, particularly for simplifying the conduct and interpretation of statistical testing but means that the severity of problems cannot be extrapolated and limits comparisons between studies. It seems counterintuitive to use a tool featuring a likert-scale to indicate the burden of HNC, only to discard this feature in the analysis and presentation of results. Where such reduction of domains is necessary, we feel that inclusion of the full domain scores as supplementary data may be helpful to complement the primary analysis. Utility values, presented alone, also result in loss of granularity. Where full domain data is available (Table 2), we find that the burden following HNC treatment is symptom-related, with a large number of patients having only mild or no functional limitations, but persistent moderate-severe pain and anxiety. This information is important as it indicates where interventions to improve QOL should be targeted for maximum impact, and has implications for commissioning support services for HNC patients. Further, because a number of studies demonstrated a ceiling effect for utility values (i.e., median scores of 1 indicating optimal health). Domain-level data would help to distinguish subgroups with persistent symptom burden despite overall good health utility.
While some trends in QOL relating to clinicopathological, sociodemographic and other factors were identified in studies, interpretation requires contextualising against the reference population. For this reason, health utility values offer insights that may otherwise be missed. For example, as was discussed by Rogers (6), while a comparison between different age groups may appear to show no difference in utility values within study cohorts, the UK reference population shows higher utility values in younger patients. Therefore, comparisons only make sense when the disparity in HRQOL between HNC cohorts and an age-matched reference population is also evaluated, as real reductions in QOL may otherwise be underestimated or missed entirely.
The majority of studies were cross-sectional in nature, with timing of HRQOL assessment varying between: at diagnosis, immediately after treatment, and various post-treatment timepoints. This makes comparisons between such studies challenging, and due to the temporal changes observed in longitudinal studies that measure across different pre and post-treatment intervals (21,24), may limit the value of such studies to inform clinical practice. The UK-wide EUROQOL assessment assesses QOL at 18 months post-diagnosis, giving a reasonable indication of the long-term HRQOL burden following treatment for HNC, but we found few studies that selected this timepoint. Although the same limitations described for cross-sectional analyses apply, a consistent post-treatment interval as is used by the EUROQOL group does provide a useful framework for establishing longer-term patient outcomes and identifying potentially unmet needs, particularly if the assessment is repeated at regular intervals to assess the impact in any changes to service provision, diagnostic or treatment pathways.
Most of the included studies evaluated patients with a primary diagnosis of HNC who were treated with curative intent, excluding those with recurrent, metastatic of palliatively treated HNC. However, we found that these latter cohorts had the greatest HRQOL deficit and are likely under-represented in research. Although recruitment of such participants may pose additional challenges and analysis can be complicated by a high mortality rate, these especially vulnerable patient cohorts represent an important subset of the HNC population and should only be excluded where justifiable and necessary. Similarly, only Davies (42) specifically enumerated the number of patients whose health utility value was <0 (i.e. a health state deemed worse than death) (25), while several studies provided ranges that clearly included <0 utility values. This cohort, although fortunately a very small proportion of HNC patients could be important to evaluate in more detail, as they are likely not appropriate for curative treatment, and so effective palliation methods to improve HRQOL are an important objective for which there is a dearth of evidence specific to HNC (25).
Perhaps surprisingly, in 12 of the 23 studies that reported health utility values, the mean plus one standard deviation includes 1 (i.e., perfect health), indicating a ceiling effect. While this is a positive finding, showing that health after HNC can return to a state equivalent to matched reference populations without HNC, it may be reflective of tendency to sample/recruit participants with less advanced disease more suitable to local surgical excision without extensive reconstruction or adjuvant treatments. In these instances, the importance of domain-specific analyses is highlighted, as further improvements can only come from the subsets of patients with problems and should be tailored towards those with the more extreme functional/symptom deficits to maximise impact. This finding may also reflect the low specificity of the EQ-5D for HNC, and it may be that the VAS offers better sensitivity for detecting the impact of these problems on patients’ QOL.
Despite being one of the most widely used HRQOL indices in cancer, few papers reported the EORTC-QLQ-C30. This index is included in the current EUROQOL national HRQOL assessment and complements the EQ-5D by including the more cancer-specific issues and concerns patients may experience, regardless of whether these appear to impact overall health or global QOL. This large-scale assessment will also enable more thorough validation of the EQ-5D and EORTC-C30 in HNC populations and specific subgroups, such as those treated palliatively, or HPV-related oropharyngeal cancers, whose demographic features differ from the majority of HPV negative HNC patients. Further implementation of these indices should be undertaken alongside HNC-specific assessments to ensure that outcomes are an accurate reflection of specific patient subsets’ needs and concerns.
This review is limited to tabular and narrative evidence synthesis, due to the high variability of studies and characteristics found. If more interventional studies are undertaken in well-defined HNC cohorts, with EQ-5D assessments undertaken at consistent intervals, it may be possible to compare these studies by meta-analysis. We also only included studies published in English language, although it should be noted that no potentially relevant studies were identified that were not available in English.
Recommendations for future research
We suggest that future research should aim to evaluate the EQ-5D alongside cancer and HNC-specific QOL indices [or alternatives to QOL indices such as the Patient Concerns Inventory (13,77)] in specific HNC cohorts, controlling for demographic, clinicopathological and treatment factors. Further validation of these disease-specific indices in different languages and cultures is important to enable better global engagement with HRQOL research in HNC patients. We observed that patient populations from Africa and South America were underrepresented in this review.
There is clear evidence that HRQOL is an important outcome for HNC research, and we see little justification to avoid including this as at least a secondary outcome in any interventional study within the field. Future researchers should plan for this either within the main patient cohort or as a sub-study.
Analysis of extreme outcomes should be considered where these exist, even if numbers are low—both indices indicating near perfect or very poor HRQOL may enable a transition toward more individualised patient-centred care and may identify important protective or deleterious factors that may influence choice of treatment, or indeed help inform clinicians and patients whether treatment is the correct option.
We found that use and reporting of the EQ-5D QOL questionnaire varied widely between studies, making comparisons between different HNC cohorts difficult. Standardised reporting criteria for EQ-5D should be developed. We recommend as a minimum that both VAS and utility values are presented, as these reflect complementary but distinct outcomes. Inclusion of full domain-level data may be appended as supplementary information, alongside more detailed analysis of extreme results, particularly if these are unexpected. The authors of this review appreciate that it may not always be feasible for these values to be presented within main study publications and would consider supplementary published material containing this data to be a valuable asset for future research.
Acknowledgments
We would like to thank Professor Simon Rogers, Professor Anastasios Kanatas and Mr. Derek Lowe for their input and feedback during the review process.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by Guest Editors (Simon N Rogers, Anastasios Kanatas) for the series “Health-Related-Quality of Life in Head and Neck Oncology” published in Frontiers of Oral and Maxillofacial Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA-ScR reporting checklist. Available at https://fomm.amegroups.com/article/view/10.21037/fomm-21-91/rc
Peer Review File: Available at https://fomm.amegroups.com/article/view/10.21037/fomm-21-91/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-21-91/coif). The series “Health-Related-Quality of Life in Head and Neck Oncology” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- UK CR. Head and neck cancer statistics 2021. Available online: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/head-and-neck-cancers
- Rogers SN, Lowe D, Lowies C, et al. Improving quality of life through the routine use of the patient concerns inventory for head and neck cancer patients: a cluster preference randomized controlled trial. BMC Cancer 2018;18:444. [Crossref] [PubMed]
- Rogers SN, Heseltine N, Flexen J, et al. Structured review of papers reporting specific functions in patients with cancer of the head and neck: 2006 - 2013. Br J Oral Maxillofac Surg 2016;54:e45-e51. [Crossref] [PubMed]
- Ghazali N, Cadwallader E, Lowe D, et al. Fear of recurrence among head and neck cancer survivors: longitudinal trends. Psychooncology 2013;22:807-13. [Crossref] [PubMed]
- Rogers SN, Allmark C, Bekiroglu F, et al. Improving quality of life through the routine use of the patient concerns inventory for head and neck cancer patients: baseline results in a cluster preference randomised controlled trial. Eur Arch Otorhinolaryngol 2020;277:3435-47. [Crossref] [PubMed]
- Rogers SN, Miller RD, Ali K, et al. Patients' perceived health status following primary surgery for oral and oropharyngeal cancer. Int J Oral Maxillofac Surg 2006;35:913-9. [Crossref] [PubMed]
- England N. The NHS Long Term Plan 2019 [14 September 2021]. Available online: https://www.longtermplan.nhs.uk/publication/nhs-long-term-plan/
- England N. Cancer Quality of Life Survey 2021. Available online: https://www.cancerqol.england.nhs.uk//
- Senchak JJ, Fang CY, Bauman JR. Interventions to improve quality of life (QOL) and/or mood in patients with head and neck cancer (HNC): a review of the evidence. Cancers Head Neck 2019;4:2. [Crossref] [PubMed]
- Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med 2018;169:467-73. [Crossref] [PubMed]
- Cocks K, Contente M, Simpson S, et al. A Q-TWiST Analysis Comparing Nivolumab and Therapy of Investigator's Choice in Patients with Recurrent/Metastatic Platinum-Refractory Squamous Cell Carcinoma of the Head and Neck. Pharmacoeconomics 2019;37:1041-7. [Crossref] [PubMed]
- Harrington KJ, Ferris RL, Blumenschein G Jr, et al. Nivolumab versus standard, single-agent therapy of investigator's choice in recurrent or metastatic squamous cell carcinoma of the head and neck (CheckMate 141): health-related quality-of-life results from a randomised, phase 3 trial. Lancet Oncol 2017;18:1104-15. [Crossref] [PubMed]
- Rogers SN, Allmark C, Bekiroglu F, et al. Improving quality of life through the routine use of the patient concerns inventory for head and neck cancer patients: main results of a cluster preference randomised controlled trial. Eur Arch Otorhinolaryngol 2021;278:3435-49. [Crossref] [PubMed]
- Noel CW, Keshavarzi S, Forner D, et al. Construct Validity of the EuroQoL-5 Dimension and the Health Utilities Index in Head and Neck Cancer. Otolaryngol Head Neck Surg 2022;166:877-85. [Crossref] [PubMed]
- Noel CW, Stephens RF, Su JS, et al. Mapping the EORTC QLQ-C30 and QLQ-H&N35, onto EQ-5D-5L and HUI-3 indices in patients with head and neck cancer. Head Neck 2020;42:2277-86. [Crossref] [PubMed]
- Del Barco Morillo E, Mesía R, Adansa Klain JC, et al. Phase II study of panitumumab and paclitaxel as first-line treatment in recurrent or metastatic head and neck cancer. TTCC-2009-03/VECTITAX study. Oral Oncol 2016;62:54-9. [Crossref] [PubMed]
- Harrington KJ, Soulières D, Le Tourneau C, et al. Quality of Life With Pembrolizumab for Recurrent and/or Metastatic Head and Neck Squamous Cell Carcinoma: KEYNOTE-040. J Natl Cancer Inst 2021;113:171-81. [Crossref] [PubMed]
- Jansen F, Coupé VMH, Eerenstein SEJ, et al. Cost-utility and cost-effectiveness of a guided self-help head and neck exercise program for patients treated with total laryngectomy: Results of a multi-center randomized controlled trial. Oral Oncol 2021;117:105306. [Crossref] [PubMed]
- Jones DA, Mistry P, Dalby M, et al. Concurrent cisplatin or cetuximab with radiotherapy for HPV-positive oropharyngeal cancer: Medical resource use, costs, and quality-adjusted survival from the De-ESCALaTE HPV trial. Eur J Cancer 2020;124:178-85. [Crossref] [PubMed]
- Mehanna H, Wong WL, McConkey CC, et al. PET-CT Surveillance versus Neck Dissection in Advanced Head and Neck Cancer. N Engl J Med 2016;374:1444-54. [Crossref] [PubMed]
- Sayed R, El Wakeel L, Saad AS, et al. Pentoxifylline and vitamin E reduce the severity of radiotherapy-induced oral mucositis and dysphagia in head and neck cancer patients: a randomized, controlled study. Med Oncol 2019;37:8. [Crossref] [PubMed]
- Truong MT, Zhang Q, Rosenthal DI, et al. Quality of Life and Performance Status From a Substudy Conducted Within a Prospective Phase 3 Randomized Trial of Concurrent Accelerated Radiation Plus Cisplatin With or Without Cetuximab for Locally Advanced Head and Neck Carcinoma: NRG Oncology Radiation Therapy Oncology Group 0522. Int J Radiat Oncol Biol Phys 2017;97:687-99. [Crossref] [PubMed]
- Amit M, Hutcheson K, Zaveri J, et al. Patient-reported outcomes of symptom burden in patients receiving surgical or nonsurgical treatment for low-intermediate risk oropharyngeal squamous cell carcinoma: A comparative analysis of a prospective registry. Oral Oncol 2019;91:13-20. [Crossref] [PubMed]
- Aoki T, Ota Y, Izawa K, et al. Correlation of preference- and profile-based quality of life of Japanese oral cancer patients during the perioperative period measured using EQ-5D-5L and FACT-H&N. Int J Oral Maxillofac Surg 2022;51:992-9. [Crossref] [PubMed]
- Lango MN, Galloway TJ, Mehra R, et al. Impact of baseline patient-reported dysphagia on acute gastrostomy placement in patients with head and neck squamous cell carcinoma undergoing definitive radiation. Head Neck 2016;38:E1318-24. [Crossref] [PubMed]
- Lango MN, Egleston B, Fang C, et al. Baseline health perceptions, dysphagia, and survival in patients with head and neck cancer. Cancer 2014;120:840-7. [Crossref] [PubMed]
- Marcellusi A, Capone A, Favato G, et al. Health utilities lost and risk factors associated with HPV-induced diseases in men and women: the HPV Italian collaborative study group. Clin Ther 2015;37:156-167.e4. [Crossref] [PubMed]
- Pottel L, Lycke M, Boterberg T, et al. G-8 indicates overall and quality-adjusted survival in older head and neck cancer patients treated with curative radiochemotherapy. BMC Cancer 2015;15:875. [Crossref] [PubMed]
- van Hinte G, Sancak T, Weijs WLJ, et al. Effect of elective neck dissection versus sentinel lymph node biopsy on shoulder morbidity and health-related quality of life in patients with oral cavity cancer: A longitudinal comparative cohort study. Oral Oncol 2021;122:105510. [Crossref] [PubMed]
- Zhang H, Xie M, Archibald SD, et al. Association of Marijuana Use With Psychosocial and Quality of Life Outcomes Among Patients With Head and Neck Cancer. JAMA Otolaryngol Head Neck Surg 2018;144:1017-22. [Crossref] [PubMed]
- ACTION Study Group. Health-related quality of life and psychological distress among cancer survivors in Southeast Asia: results from a longitudinal study in eight low- and middle-income countries. BMC Med 2017;15:10. [Crossref] [PubMed]
- Aoki T, Ota Y, Sasaki M, et al. To what extent does the EQ-5D-3L correlate with the FACT-H&N of patients with oral cancer during the perioperative period? Int J Clin Oncol 2019;24:350-8. [Crossref] [PubMed]
- Beck ACC, Kieffer JM, Retèl VP, et al. Mapping the EORTC QLQ-C30 and QLQ-H&N35 to the EQ-5D for head and neck cancer: Can disease-specific utilities be obtained? PLoS One 2019;14:e0226077. [Crossref] [PubMed]
- Maximiano C, López I, Martín C, et al. An exploratory, large-scale study of pain and quality of life outcomes in cancer patients with moderate or severe pain, and variables predicting improvement. PLoS One 2018;13:e0193233. [Crossref] [PubMed]
- Plaschke CC, Bertino G, McCaul JA, et al. European Research on Electrochemotherapy in Head and Neck Cancer (EURECA) project: Results from the treatment of mucosal cancers. Eur J Cancer 2017;87:172-81. [Crossref] [PubMed]
- Sprave T, Zamboglou C, Verma V, et al. Characterization of health-related quality of life based on the EQ-5D-5L questionnaire in head-and-neck cancer patients undergoing modern radiotherapy. Expert Rev Pharmacoecon Outcomes Res 2020;20:673-82. [Crossref] [PubMed]
- Tsai YT, Chen WC, Hsu CM, et al. Survival-Weighted Health Profiles in Patients Treated for Advanced Oral Cavity Squamous Cell Carcinoma. Front Oncol 2021;11:754412. [Crossref] [PubMed]
- Baxi SS, Salz T, Xiao H, et al. Employment and return to work following chemoradiation in patient with HPV-related oropharyngeal cancer. Cancers Head Neck 2016;1:4. [Crossref] [PubMed]
- Baxi SS, Cullen G, Xiao H, et al. Long-term quality of life in older patients with HPV-related oropharyngeal cancer. Head Neck 2018;40:2321-8. [Crossref] [PubMed]
- Broderick D. How much of a problem is too much saliva for patients following head and neck cancer. Br J Oral Maxillofac Surg 2020;58:e51-6. [Crossref] [PubMed]
- Cardoso RC, Kamal M, Zaveri J, et al. Self-Reported Trismus: prevalence, severity and impact on quality of life in oropharyngeal cancer survivorship: a cross-sectional survey report from a comprehensive cancer center. Support Care Cancer 2021;29:1825-35. [Crossref] [PubMed]
- Davies A, Waylen A, Leary S, et al. Assessing the validity of EQ-5D-5L in people with head & neck cancer: Does a generic quality of life measure perform as well as a disease-specific measure in a patient population? Oral Oncol 2020;101:104504. [Crossref] [PubMed]
- Giuliani M, Papadakos J, Broadhurst M, et al. The prevalence and determinants of return to work in head and neck cancer survivors. Support Care Cancer 2019;27:539-46. [Crossref] [PubMed]
- Jansen F, Coupé VMH, Eerenstein SEJ, et al. Costs from a healthcare and societal perspective among cancer patients after total laryngectomy: are they related to patient activation? Support Care Cancer 2018;26:1221-31. [Crossref] [PubMed]
- Anderson Head MDNeck Cancer Symptom Working Group. Patient reported dry mouth: Instrument comparison and model performance for correlation with quality of life in head and neck cancer survivors. Radiother Oncol 2018;126:75-80. [Crossref] [PubMed]
- Karczewska-Lindinger M, Tuomi L, Fridolfsson J, et al. Low physical activity in patients diagnosed with head and neck cancer. Laryngoscope Investig Otolaryngol 2021;6:747-55. [Crossref] [PubMed]
- Khadela A, Vyas B, Bhikadiya V, et al. Impact of clinical pharmacist services on quality adjusted life years in head and neck cancer patients. Int J Clin Pharm 2021;43:1208-17. [Crossref] [PubMed]
- Kimman M, Jan S, Monaghan H, et al. The relationship between economic characteristics and health-related quality of life in newly diagnosed cancer patients in Southeast Asia: results from an observational study. Qual Life Res 2015;24:937-49. [Crossref] [PubMed]
- Kularatna S, Whitty JA, Johnson NW, et al. A comparison of health state utility values associated with oral potentially malignant disorders and oral cancer in Sri Lanka assessed using the EQ-5D-3 L and the EORTC-8D. Health Qual Life Outcomes 2016;14:101. [Crossref] [PubMed]
- Lastrucci L, Bertocci S, Bini V, et al. Late toxicity, evolving radiotherapy techniques, and quality of life in nasopharyngeal carcinoma. Radiol Med 2017;122:303-8. [Crossref] [PubMed]
- McDowell LJ, Rock K, Xu W, et al. Long-Term Late Toxicity, Quality of Life, and Emotional Distress in Patients With Nasopharyngeal Carcinoma Treated With Intensity Modulated Radiation Therapy. Int J Radiat Oncol Biol Phys 2018;102:340-52. [Crossref] [PubMed]
- Noel CW, Lee DJ, Kong Q, et al. Comparison of Health State Utility Measures in Patients With Head and Neck Cancer. JAMA Otolaryngol Head Neck Surg 2015;141:696-703. [Crossref] [PubMed]
- Obeso-Benítez P, Muñoz-Vigueras N, Castillo-Pérez I, et al. Global functional impairment in head and neck cancer survivors after completing radiotherapy treatment. Disabil Rehabil 2022;44:6394-400. [Crossref] [PubMed]
- Pickard AS, Jiang R, Lin HW, et al. Using Patient-reported Outcomes to Compare Relative Burden of Cancer: EQ-5D and Functional Assessment of Cancer Therapy-General in Eleven Types of Cancer. Clin Ther 2016;38:769-77. [Crossref] [PubMed]
- Ramaekers BL, Joore MA, Grutters JP, et al. The impact of late treatment-toxicity on generic health-related quality of life in head and neck cancer patients after radiotherapy. Oral Oncol 2011;47:768-74. [Crossref] [PubMed]
- Setiawan D, Dusafitri A, Galistiani GF, et al. Health-Related Quality of Life of Patients with HPV-Related Cancers in Indonesia. Value Health Reg Issues 2018;15:63-9. [Crossref] [PubMed]
- Singh P, Bennett B, Bailey T, et al. Real-world study of the impact of recurrent/metastatic squamous cell carcinoma of the head and neck (R/M SCCHN) on quality of life and productivity in Europe. BMC Cancer 2021;21:854. [Crossref] [PubMed]
- Singh P, Contente M, Bennett B, et al. Real-World Treatment Patterns and Outcomes in Patients with Head and Neck Cancer: Point-in-Time Survey of Oncologists in Italy and Spain. Adv Ther 2021;38:4722-35. [Crossref] [PubMed]
- Stephens RF, Noel CW, Su JS, et al. Mapping the University of Washington Quality of life questionnaire onto EQ-5D and HUI-3 indices in patients with head and neck cancer. Head Neck 2020;42:513-21. [Crossref] [PubMed]
- Thankappan K, Patel T, Ajithkumar KK, et al. Mapping of head and neck cancer patient concerns inventory scores on to Euroqol-Five Dimensions-Five Levels (EQ-5D-5L) health utility scores. Eur J Health Econ 2022;23:225-35. [Crossref] [PubMed]
- Tyler MA, Mohamed ASR, Smith JB, et al. Long-term quality of life after definitive treatment of sinonasal and nasopharyngeal malignancies. Laryngoscope 2020;130:86-93. [Crossref] [PubMed]
- Lai CH, Chen WC, Fang CC, et al. Survival-Weighted Health Profiles in Nasopharyngeal Cancer Patients. Front Oncol 2021;11:635667. [Crossref] [PubMed]
- Lai WW, Chung CH, Lin CN, et al. QALYs and medical costs saved from prevention of a cancer: Analysis of nation-wide real-world data of Taiwan with lifetime horizon. J Formos Med Assoc 2021;120:2089-99. [Crossref] [PubMed]
- van der Linden N, Flach GB, de Bree R, et al. Cost-utility of sentinel lymph node biopsy in cT1-T2N0 oral cancer. Oral Oncol 2016;53:20-6. [Crossref] [PubMed]
- Bäuerle A, Musche V, Schmidt K, et al. Mental Health Burden of German Cancer Patients before and after the Outbreak of COVID-19: Predictors of Mental Health Impairment. Int J Environ Res Public Health 2021;18:2318. [Crossref] [PubMed]
- Chan KK, Willan AR, Gupta M, et al. Underestimation of uncertainties in health utilities derived from mapping algorithms involving health-related quality-of-life measures: statistical explanations and potential remedies. Med Decis Making 2014;34:863-72. [Crossref] [PubMed]
- Deckard NA, Harrow BR, Barnett SL, et al. Comparative analysis of quality-of-life metrics after endoscopic surgery for sinonasal neoplasms. Am J Rhinol Allergy 2015;29:151-5. [Crossref] [PubMed]
- Gao F, Ng GY, Cheung YB, et al. The Singaporean English and Chinese versions of the EQ-5D achieved measurement equivalence in cancer patients. J Clin Epidemiol 2009;62:206-13. [Crossref] [PubMed]
- Heutte N, Plisson L, Lange M, et al. Quality of life tools in head and neck oncology. Eur Ann Otorhinolaryngol Head Neck Dis 2014;131:33-47. [Crossref] [PubMed]
- Jansen F, Krebber AM, Coupé VM, et al. Cost-Utility of Stepped Care Targeting Psychological Distress in Patients With Head and Neck or Lung Cancer. J Clin Oncol 2017;35:314-24. [Crossref] [PubMed]
- Krebber AM, Leemans CR, de Bree R, et al. Stepped care targeting psychological distress in head and neck and lung cancer patients: a randomized clinical trial. BMC Cancer 2012;12:173. [Crossref] [PubMed]
- Meregaglia M, Cairns J. A systematic literature review of health state utility values in head and neck cancer. Health Qual Life Outcomes 2017;15:174. [Crossref] [PubMed]
- Mozzanica F, Scarponi L, Rota M, et al. Psychometric properties of the Italian version of the Speech Handicap Index. Disabil Rehabil 2021;43:1307-12. [Crossref] [PubMed]
- Nichols AC, Lang P, Prisman E, et al. Treatment de-escalation for HPV-associated oropharyngeal squamous cell carcinoma with radiotherapy vs. trans-oral surgery (ORATOR2): study protocol for a randomized phase II trial. BMC Cancer 2020;20:125. [Crossref] [PubMed]
- Ryu M, Hwang JI. Cancer site differences in the health-related quality of life of Korean cancer survivors: Results from a Population-based Survey. Public Health Nurs 2019;36:144-54. [Crossref] [PubMed]
- Schwarzinger M, Luchini SEPICORL Study Group. Estimating health state utility from activities of daily living in the French National Hospital Discharge Database: a feasibility study with head and neck cancer. Health Qual Life Outcomes 2019;17:129. [Crossref] [PubMed]
- Miller N, Rogers SN. A review of question prompt lists used in the oncology setting with comparison to the Patient Concerns Inventory. Eur J Cancer Care (Engl) 2018; [Crossref] [PubMed]
Cite this article as: Walshaw EG, Thom L, Boyes H, Twigg J. A scoping review of utilisation of the EQ-5D questionnaire to evaluate health-related quality of life following a diagnosis of head and neck cancer. Front Oral Maxillofac Med 2024;6:7.

