
Surgery first orthognathic approach: a case series of 3D planning and pre-bent plates in patients with single- and double-jaw surgeries
Highlight box
Key findings
• 3D planning and pre-bent plates decrease operative time, increase operative accuracy, and have comparable results at long-term follow-up compared to conventional methods.
What is known and what is new?
• Surgery first orthognathic approach (SFOA) involves performing surgery prior to orthodontics and is indicated for specific cases. Virtual surgical planning (VSP) supplants traditional planning methods with plaster models by utilizing 3D computerized technology and allowing the creation of customized patient-specific pre-bent plates.
• Application of VSP and pre-bent plates to surgery first orthognathic cases where surgeons may lack occlusion to guide intraoperative movements improves accuracy and reduces operative time.
What is the implication, and what should change now?
• VSP in SFOA should be accepted as a potentially superior method to traditional methods, though further research is needed to justify its increased training time and evaluate for its applicability to a wider variety of orthognathic cases.
Introduction
Background
Orthodontic and orthognathic surgery improves facial anatomy, esthetics, and function in patients with dentofacial deformities (1). Since Dr. Hugo Obwegeser’s introduction of the Le Fort I osteotomy in the 1950s, orthognathic surgery has become a mainstay of craniomaxillofacial surgery. Traditionally, an “orthodontics-first” approach consisting of preoperative orthodontics followed by surgery and postoperative orthodontics was the accepted approach to reconstructive jaw surgery (2,3).
However, recently a “surgery-first” approach to orthognathic surgery has introduced a new treatment paradigm for the management of dentomaxillofacial deformities (1,3,4). This “surgery-first” approach is currently indicated for treatment of obstructive sleep apnea (OSA), class III deformities, and facial asymmetry (1). Overall treatment time is 25% to 50% shorter in the surgery-first approach compared to the traditional approach, in part due to the reduced duration of orthodontic treatment compared to patients that receive traditional preoperative and postoperative orthodontic treatment (1,5).
While pre-operative orthodontic time is eliminated, postoperative orthodontic time is also frequently reduced due in part to the partial resolution of dentoalveolar compensation following surgery. Additionally, correction of the skeletal base discrepancy allows the direction of postsurgical treatment to coincide with natural dental compensation and muscular force, resulting in decreased time to full compensation and reduced complexity of postoperative orthodontic treatment (5). Moreover, as surgery-first protocols produce immediate improvement of the facial profile and upper airway constriction for patients, they generally improve patient satisfaction, patient compliance, and overall outcomes during postoperative orthodontics (6).
The method of preparing a patient for orthognathic surgery has also been revolutionized by the adoption of preoperative 3D planning (7). Traditionally, preparation for orthognathic surgery implemented panoramic or posterior anterior 2D images, paper planning, and creation of plaster models mounted on semi-adjustable articulators (8). Prior to the advent of 3D planning, these plaster models were used to simulate surgery and create surgical splints, a process that was laborious, time-consuming, and often resulted in inaccuracies (9).
However, the development of 3D computerized technology enabled the creation of a computer-aided design/computer-aided manufacturing (CAD/CAM) and virtual surgical planning (VSP) to create individualized models of each patient’s skulls from preoperative computed tomography (CT) scans (10,11). VSP enables fabrication of drilling guide templates and pre-bent titanium plates that can be manufactured and printed utilizing CAD/CAM technologies (12,13). These models allow for the ability to perform virtual surgeries or to create surgical osteotomy guides, occlusal splints, spacers, and pre-bent plates that can be applied intraoperatively (8,13). This technology has been demonstrated to not only reduce surgical time, but also improve operative accuracy (12-14).
Rationale and knowledge gap
Although pre-bent plates are widely accepted in trauma and reconstructive surgery, evidence for the efficacy of pre-bent plates in orthognathic surgery is more limited (15). Studies have shown that the use of 3D planning, cutting and drilling guides and pre-bent titanium plates can accurately transfer a virtual plan to the operating room in Le Fort I osteotomies and bilateral sagittal split osteotomies (BSSO) for skeletal class II deformities and anterior open bite, but the appropriateness and feasibility of widespread adoption for all orthognathic cases is still in question (16).
Objective
In this case series report, we share our institution’s experience with the implementation of 3D planning and pre-bent plates into orthognathic surgery in a series of case reports. We present this article in accordance with the AME Case Series reporting checklist (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-76/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case series and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Patient 1
A 21-year-old Hispanic male with no significant past medical or surgical history presented with a chief complaint of difficulty eating and associated pain in the temporomandibular joint (TMJ) bilaterally during mastication. Patient had undergone orthodontic treatment 5 years prior and now was referred by their orthodontist for assessment and management of the malocclusion and the patient’s bilateral joint pain.
On clinical examination, the patient’s maxilla was noted to be anteroposterior (AP) deficient because of significant maxillary hypoplasia with skeletal class III malocclusion complicated by severe TMJ pain (17). Patient was noted to have 9 mm of negative overjet, 4 mm of overbite, bilateral posterior crossbite, no upper incisal show at rest, and a maximum interincisal opening (MIO) of 55 mm. On intra-oral examination, the mandibular dental midline was coincident with the facial midline, while the maxillary dental and skeletal midline was approximately 2 mm deviated to the right (Figure 1).

Functional assessment revealed difficulty masticating due to inability to use anterior teeth, bilateral TMJ pain and popping with mastication with more severe symptoms on the right side, and a lisp for which the patient reported prior speech therapy as a child.
The patient underwent VSP using ProplanCMF software (DePuy Synthes, USA) in which a 1-piece Le Fort I advancement of 6 mm, rotation of 1 mm to the left to correct the midline, and 5 mm down grafting was planned. A 6 mm setback was planned for the mandible, with no alteration to the dental or skeletal midline. Custom surgical cutting guides, intermediate and final occlusal splints, and custom patient-specific titanium plates were fabricated by DePuy Synthes. There were no intraoperative complications with any 3D printed/pre-bent plates and splints were highly accurate.
Patient was placed into heavy elastics for a period of 2 weeks, thereafter the elastics were progressively lightened. Orthodontic treatment was initiated 6 weeks post-operatively. Duration of orthodontic treatment was 8.5 months. A skeletal and dental class I occlusion was achieved, with improved mastication and speech as well as an improvement of patient’s TMJ symptoms (Figures 2,3A,3B).


Patient 2
A 32-year-old Hispanic male with a medical history significant for diabetes mellitus, major depressive disorder, hyperlipidemia, obesity, and generalized anxiety disorder was referred by a dentist for evaluation of his malocclusion. The patient had orthodontic treatment 6 years prior to presentation. He reported difficulty masticating and bilateral TMJ pain on opening and mastication.
On extraoral examination, the patient demonstrated maxillary AP deficiency with a significant skeletal and dental class III malocclusion; the patient also appeared vertically deficient in the middle 1/3 (Figure 4). He had a significant concavity on profile and marked paranasal flattening on frontal view.

Intraoral exam revealed a bilateral posterior and anterior crossbite, 7 mm negative overjet, 3 mm overbite, MIO of 55 mm, no third molars, no maxillary incisal show at rest and multiple diastemas in maxilla and mandible. The maxillary midline was coincident with the facial midline, and the mandibular and chin midline deviated 2 mm to the left.
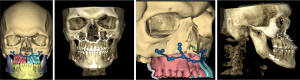
Following study models, imaging, and a treatment discussion with the orthodontist, a surgery-first orthognathic approach (SFOA) with a 2-piece Le Fort I and BSSO osteotomy was planned. VSP was performed using ProplanCMF software (DePuy Synthes). Custom cutting guides, intermediate and final occlusal splints, and patient-specific titanium plates were fabricated by DePuy Synthes.
The patient underwent a 2-piece Le Fort I osteotomy with a 7 mm maxillary advancement, down graft of 1 mm, a mid-palatal split, and widening of the upper arch by 1.6 mm. The mandible was rotated 10° clockwise, with a resultant 0.7 mm overlap at proximal cut lingually (Figure 5). The patient’s final splint was wired into the post-treatment occlusion and the patient was placed into heavy elastics.
No complications arose during the procedure, and the patient was discharged 24 hours postoperatively. Orthodontic treatment was initiated 4 weeks postoperatively to address the spacing and reduce flaring of the upper anterior maxillary teeth. The palatal splint was removed at 8 weeks postoperatively. At 3 months postoperatively, extraoral examination revealed a skeletal class I relationship with a planned class II dental relationship (Figure 6A). Orthodontic treatment was completed after 6 months with a final dental class I relationship (Figure 6B). Patient has reported a persistent reciprocal click on mouth opening with no pain or deviation on opening.

Patient 3
A 40-year-old Hispanic female presented with a history of longstanding pain, limited mouth opening, and degenerative joint disease of bilateral TMJ that led to development of retrognathia and an anterior open bite. The patient’s medical history is significant for systemic lupus erythematosus (SLE) treated with long-term prednisone, azathioprine, and hydroxychloroquine.
Four years prior to pre-surgical assessment, the patient presented to the Oral and Maxillofacial Surgery (OMFS) clinic with severe bilateral TMJ pain and apertognathia (5 mm) secondary to chronic advanced SLE. The patient failed to return for treatment. According to the patient, she had no prior history of orthodontic treatment, but her prior dental records confirmed that she had both a skeletal and dental class I relationship prior to her diagnosis of SLE.
At pre-surgical assessment, the patient reported issues with mastication, speech distortion, fractured teeth, sleep-disordered breathing, daytime fatigue, and TMJ pain.
On extraoral examination, the patient presented with marked mandibular retrognathia, anterior open bite, maxillary and mandibular midlines congruent with each other and facial midlines, and a skeletal class II malocclusion requiring surgical intervention (Figure 7A,7B).

Intraoral exam revealed limited mouth opening at 20 mm inter-incisal distance and dentition grossly intact with malposed third molars. The treatment plan included pre-surgical orthodontic assessment, extraction of all wisdom teeth, and bilateral coronoidectomies with bilateral total joint replacement, Le Fort I osteotomy, and a genioplasty (Figure 8).

The patient was optimized by rheumatologist for surgery, and per their request, azathioprine was withheld for 1 week pre-operatively and restarted 2 weeks after surgery. Prednisone was converted to dexamethasone post-operatively, and hydroxychloroquine was held on day of surgery and resumed on post-op day 2 per the rheumatologist’s recommendations. She was placed in orthodontic brackets 7 days prior to surgery.
Intraoperatively there were no complications, and a stable tripod occlusion was obtained. Healing was uneventful, and orthodontic treatment was initiated 7 weeks post-op to address persistent maxillary spacing and slight planned anterior open bite (Figure 9). Duration of orthodontic treatment was 6 months with a stable dental and skeletal class 1 relationship at 18 months post completion of treatment.

Patient 4
A 48-year-old Hispanic male with no significant past medical history was referred for evaluation due to complaints of malocclusion. Four months prior to referral to OMFS, the patient suffered a right mandibular sub condylar fracture from a work-related injury. Patient underwent closed reduction with maxillomandibular fixation for 6 weeks for treatment of right sub condylar fracture by another surgical discipline.
The patient presented to our clinic complaining of a right premature contact, mandibular midline deviation to the right side, persistent right sided joint pain, and difficulty with mastication. Pretreatment assessment revealed anterior open bite of 3 mm, dental class III malocclusion with right posterior crossbite, maxillary transverse deficiency and MIO of 35 mm (Figure 10).

His orthodontist did an evaluation and agreed with SFOA for treatment. VSP was performed using ProplanCMF software (DePuy Synthes) for a 3-piece Le Fort I osteotomy (Figure 11). Orthodontic brackets were placed 7 days prior to surgery.
There were no complications intraoperatively, and the patient was discharged on post-op day one. On post-op day 7, the patient was readmitted to the hospital for persistent right-sided epistaxis, requiring embolization of right sphenopalatine artery by interventional radiology and discharged 2 days later.
Post-treatment images at 4 weeks (Figure 12A) and at 7 weeks (Figure 12B) demonstrate class I molar and canine occlusion. At 7 weeks post-op, palatal splint was removed, and orthodontic treatment initiated.

The patient demonstrated improved facial projection as well as the predicted upper incisor show at 27 weeks post-op (Figure 12C). The patient completed his orthodontic treatment 9 months after the surgery was completed.
Discussion
Key findings
In our experience with VSP, we observed: (I) there was no or negligible difference in the accuracy of VSP when planning for SFOA in patients with either class II or III malocclusion, (II) VSP predictability and accuracy was similar when comparing single or double jaw surgeries, (III) 2 to 3 piece Le Fort I VSP appointments required increased planning time due to lack of stable initial occlusion but had no negative outcomes nor inaccuracies on final splints and 3D models (18-20).
Explanation of findings & comparison with similar researches
Based on our experiences in post-obliterative and reconstruction surgery, there was a gradual progression to the use of pre-bent plates in traditional orthognathic surgery followed by SFOA with similar stable long term follow-up results. These results are compatible with Badiali’s study which showed highly satisfactory results using pre-bent plates in orthognathic surgery (20). The use of pre-bent plates is closely tied to the accuracy of the 3D planning step, especially when adopting SFOA in a single jaw due to the lack of predictable and reproducible occlusion as guide for final jaw position.
In our experience, use of pre-bent plates for Le Fort I osteotomies not only significantly reduced operative time, but also provided a higher degree of accuracy and predictability regardless of the vector or amount of maxillary movement (13). In all our cases, a printed occlusal splint was secured prior to plating with the pre-bent plates. Additionally, the advancement of technology and surgical techniques allowed fabrication of printed cutting guides with pre-drilling fixation holes for use prior to down fracturing of the maxilla (12-14).
Even in SFOA cases, the accuracy of the cutting guides and pre-bent plates allowed the surgeon to fixate the maxilla without prior splint insertion. The splint could be inserted after fixation to verify occlusion with planned occlusion. While insertion of the splint prior to plating in SFOA is still recommended, omittance is dependent on surgeon level of experience and comfort. However, when a multiple piece maxilla is planned, insertion of the splint is imperative due to the numerous possible vectors involved with multiple piece Le Fort I osteotomies (20).
Our long-term follow-up with Le Fort I osteotomies using 3D planning and pre-bent plates has demonstrated comparable long-term stability with traditional approaches (13-15). While the aforementioned technological advancements are a major contributing factor, successful orthodontic completion of the cases by the orthodontist involved is crucial.
In complex surgical cases incorporating TMJ replacement surgery and SFOA, the surgical planning required increased logistical planning and appointment length. The logistical challenge was primarily because different companies were used to create the patient-specific implants (PSI) for the joint replacement and SFOA surgeries. Although literature is lacking for combined joint replacement and SFOA, it has been shown that combined joint replacement and traditional orthodontic first orthognathic surgery using PSI provide efficient and beneficial outcomes for patients (21).
Our experience comparing the use of VSP in SFOA and traditional approaches during a BSSO have been like that with Le Fort I osteotomies. Regarding BSSO, the accuracy of the splint is essential as the pre-bent or printed plates are not as dependable as for Le Fort I osteotomies (14,22). In our initial experience, performing BSSO advancement with SFOA cases using pre-bent and printed plates did not demonstrate an advantage over traditional approaches. In fact, in one third of early SFOA cases undergoing BSSO advancement the pre-bent plates were not sufficiently long enough to allow adequate fixation on the distal segment. In these cases, we resorted to the contouring standard 1.4 mm plates.
We were able to overcome this by not only modifying the printed cutting guides to include all osteotomy cuts as opposed to just the lower border osteotomy site, but also adding a shoulder to accurately achieve a horizontal cut with correct positioning of the nerve. We also increased the length of the pre-bent plates through addition of a fixation hole in the distal segment. Such modifications to pre-bent plates prior to use for BSSO are consistent with the literature (14,22). Our experience aligns with the findings of Shakoori et al., which concluded that use of custom mandibular hardware demonstrated higher variability compared to the maxilla (22).
Importantly, recurrence rates did not differ when custom pre-bent plates were used compared to traditional plates fashioned in the operating room. The average mean post-surgical time was 8 months with no reported cases of relapse. Similarly, duration of postoperative orthodontics treatment did not differ, though shorter treatment durations have been reported for SFOA in the literature (1). However, the operative time was significantly reduced by an average of 75 minutes with the use of pre-bent plates, consistent with current literature (23).
Strengths and limitations
As an academic institution of higher education, the department of oral and maxillofacial surgery based at the largest community hospital in the Texas Medical Center has continually evolved and followed the proven current trends in the surgical management of malocclusions, together with dedicated support of the orthodontist.
Traditional surgical planning (TSP) involved lateral cephalometric analysis using Steiner’s Analysis, followed by model surgery, and visual treatment objectives. This allowed for production of intermediate and final surgical guide splints for the proposed pre-determined movements and fixation of the osteotomized segments with traditional plates which were contoured intra-operatively. Before the advent of VSP, TSP required substantial time for preoperative planning and intraoperative surgical time to achieve the desired outcome (24,25). Our migration from the traditional approach has decreased the total working time spent in double-jaw surgeries while maintaining efficacy (24,25). A principle we have maintained is that irrespective of what advances were incorporated into our pre-surgical planning and operative techniques, we would continue to ensure that traditional approaches to planning and surgery were taught, as these original protocols have well established predictability and long-term stability (24).
As our clinical practice and modalities evolved and incorporated planning software into our treatment protocols, we determined that similar predictable results with long term stability were achieved with VSP compared to TSP (26). Because VSP had been used in various reconstruction cases with improved accuracy at our institution, we were able to incorporate VSP into orthognathic surgery cases early (18). However, there exists a significant learning curve involved with planning, which is dependent on the desired plating system and planning company. As there is no obvious occlusion to guide the movements of the mandible, proper communication between the surgeon and technician performing the planning is essential to ensure the simulated movements will produce the final desired occlusion by the orthodontist (11). Finalization of the mandible position is required before an agreement can be made regarding intermediate or final splint, depending on whether single versus double jaw surgery will be performed.
Independent of the surgical planning outcome, a common finding among the various providers using VSP was the variability in the understanding of what movements were surgically achievable when following the fundamental anatomical and biological principles. The length of a successful surgical planning appointment with a software technician depended on the experience of the surgeon and the software technician (11,17). In addition, we found that more experienced surgeons and software technicians required minimal re-planning in the final stages prior to printing of the PSI and models.
There are several different skeletal and dental relationships possible on patients who would be presenting for orthognathic surgery, whilst we have tried to demonstrate a variety of different cases, it in no way encompasses the entire spectrum. Similarly, we have demonstrated various surgeries with positive outcomes, another limitation would be it does not represent all the possible vectors and magnitude of the movements possible amongst the different surgical procedures.
Implications and actions needed
Initially, VSP was used for all traditional orthognathic surgery cases prior to incorporation into cases qualified for SFOA. In our experience, use of VSP for both traditional orthognathic approach and SFOA has proven to be highly accurate and has not led to an increase in misdiagnosis nor improper planning (3,8,27,28). Based on our findings, VSP should be accepted and taught as an effective method for planning SFOA cases. However, further research is warranted to (I) investigate whether VSP and pre-bent plates is indicated in all orthognathic surgeries or only certain operations and (II) to justify that its implementation is worth the additional cost and training time.
Conclusions
Incorporating 3D planning and pre-bent plates provides benefits in treating SFOA cases by both significantly reducing operative time and adding greater accuracy in situations when the operating surgeons lack occlusion to guide intraoperative movements. While there will always be a learning curve when incorporating innovative technology into long-stand surgical procedures, our experience agrees with the literature that the use of pre-bent plates and 3D planning is both effective and time efficient.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Chung H. Kau) for the series “Managing Craniofacial and Dentofacial Disorders—Simplified Solutions for Difficult Situations” published in Frontiers of Oral and Maxillofacial Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the AME Case Series reporting checklist. Available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-76/rc
Peer Review File: Available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-76/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-76/coif). The series “Managing Craniofacial and Dentofacial Disorders—Simplified Solutions for Difficult Situations” was commissioned by the editorial office without any funding or sponsorship. C.B.P. reports that he receives consulting fee from MedCAD company. The company MedCAD does planning and pre-bent plates, however they were not one of the service providers used in the article as well as well C.B.P.’s consulting agreement is for total joint replacement services and not SOFA cases. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case series and accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Choi JW, Bradley JP. Surgery First Orthognathic Approach Without Presurgical Orthodontic Treatment: Questions and Answers. J Craniofac Surg 2017;28:1330-3. [Crossref] [PubMed]
- Huang CS, Hsu SS, Chen YR. Systematic review of the surgery-first approach in orthognathic surgery. Biomed J 2014;37:184-90. [Crossref] [PubMed]
- Peiró-Guijarro MA, Guijarro-Martínez R, Hernández-Alfaro F. Surgery first in orthognathic surgery: A systematic review of the literature. Am J Orthod Dentofacial Orthop 2016;149:448-62. [Crossref] [PubMed]
- Jung J, Moon SH, Kwon YD. Current status of surgery-first approach (part III): the use of 3D technology and the implication in obstructive sleep apnea. Maxillofac Plast Reconstr Surg 2020;42:1. [Crossref] [PubMed]
- Liao YF, Chiu YT, Huang CS, et al. Presurgical orthodontics versus no presurgical orthodontics: treatment outcome of surgical-orthodontic correction for skeletal class III open bite. Plast Reconstr Surg 2010;126:2074-83. [Crossref] [PubMed]
- Hernández-Alfaro F, Guijarro-Martínez R, Peiró-Guijarro MA. Surgery first in orthognathic surgery: what have we learned? A comprehensive workflow based on 45 consecutive cases. J Oral Maxillofac Surg 2014;72:376-90. [Crossref] [PubMed]
- Zinser MJ, Sailer HF, Ritter L, et al. A paradigm shift in orthognathic surgery? A comparison of navigation, computer-aided designed/computer-aided manufactured splints, and "classic" intermaxillary splints to surgical transfer of virtual orthognathic planning. J Oral Maxillofac Surg 2013;71:2151.e1-21. [Crossref] [PubMed]
- Tondin GM, Leal MOCD, Costa ST, et al. Evaluation of the accuracy of virtual planning in bimaxillary orthognathic surgery: a systematic review. Br J Oral Maxillofac Surg 2022;60:412-21. [Crossref] [PubMed]
- Lartizien R, Zaccaria I, Noyelles L, et al. Quantification of the inaccuracy of conventional articulator model surgery in Le Fort 1 osteotomy: evaluation of 30 patients controlled by the Orthopilot® navigation system. Br J Oral Maxillofac Surg 2019;57:672-7. [Crossref] [PubMed]
- Swennen GR, Mollemans W, Schutyser F. Three-dimensional treatment planning of orthognathic surgery in the era of virtual imaging. J Oral Maxillofac Surg 2009;67:2080-92. Erratum in: J Oral Maxillofac Surg 2009;67:2703. [Crossref] [PubMed]
- Antonini F, Borba AM, Pagnoncelli RM, et al. Does a learning curve exist for accuracy in three-dimensional planning for maxillary positioning in bimaxillary orthognathic surgery? Int J Oral Maxillofac Surg 2020;49:787-93. [Crossref] [PubMed]
- Hu P, Li J, Du W, et al. The Drilling Guiding Templates and Pre-Bent Titanium Plates Improves the Operation Accuracy of Orthognathic Surgery With Computer-Aided Design and Computer-Aided Manufacturing Occlusal Splints for Patients With Facial Asymmetry. J Craniofac Surg 2019;30:2144-8. [Crossref] [PubMed]
- Chen Z, Mo S, Fan X, et al. A Meta-analysis and Systematic Review Comparing the Effectiveness of Traditional and Virtual Surgical Planning for Orthognathic Surgery: Based on Randomized Clinical Trials. J Oral Maxillofac Surg 2021;79:471.e1-471.e19. [Crossref] [PubMed]
- Suojanen J, Leikola J, Stoor P. The use of patient-specific implants in orthognathic surgery: A series of 30 mandible sagittal split osteotomy patients. J Craniomaxillofac Surg 2017;45:990-4. [Crossref] [PubMed]
- Du W, Chen G, Bai D, et al. Treatment of skeletal open bite using a navigation system: CAD/CAM osteotomy and drilling guides combined with pre-bent titanium plates. Int J Oral Maxillofac Surg 2019;48:502-10. [Crossref] [PubMed]
- Liu S, Li J, Xu C, et al. Effect of computer-assisted design and manufacturing cutting and drilling guides accompanied with pre-bent titanium plates on the correction of skeletal class II malocclusion: a randomized controlled trial. Int J Oral Maxillofac Surg 2021;50:1320-8. [Crossref] [PubMed]
- Gravely JF, Johnson DB. Angle's classification of malocclusion: an assessment of reliability. Br J Orthod 1974;1:79-86. [Crossref] [PubMed]
- Hammoudeh JA, Howell LK, Boutros S, et al. Current Status of Surgical Planning for Orthognathic Surgery: Traditional Methods versus 3D Surgical Planning. Plast Reconstr Surg Glob Open 2015;3:e307. [Crossref] [PubMed]
- Steinhuber T, Brunold S, Gärtner C, et al. Is Virtual Surgical Planning in Orthognathic Surgery Faster Than Conventional Planning? A Time and Workflow Analysis of an Office-Based Workflow for Single- and Double-Jaw Surgery. J Oral Maxillofac Surg 2018;76:397-407. [Crossref] [PubMed]
- Badiali G, Bevini M, Lunari O, et al. PSI-Guided Mandible-First Orthognathic Surgery: Maxillo-Mandibular Position Accuracy and Vertical Dimension Adjustability. J Pers Med 2021;11:1237. [Crossref] [PubMed]
- Gomez NL, Boccalatte LA, Lopez Ruiz Á, et al. Total Temporomandibular Joint Replacement and Simultaneous Orthognathic Surgery Using Computer-Assisted Surgery. J Maxillofac Oral Surg 2021;20:394-403. [Crossref] [PubMed]
- Shakoori P, Yang R, Nah HD, et al. Computer-aided Surgical Planning and Osteosynthesis Plates for Bimaxillary Orthognathic Surgery: A Study of 14 Consecutive Patients. Plast Reconstr Surg Glob Open 2022;10:e4609. [Crossref] [PubMed]
- Ji H, Du W, Xu C, et al. Computer-assisted osteotomy guides and pre-bent titanium plates improve the planning for correction of facial asymmetry. Int J Oral Maxillofac Surg 2019;48:1043-50. [Crossref] [PubMed]
- Kwon TG, Choi JW, Kyung HM, et al. Accuracy of maxillary repositioning in two-jaw surgery with conventional articulator model surgery versus virtual model surgery. Int J Oral Maxillofac Surg 2014;43:732-8. [Crossref] [PubMed]
- Alkaabi S, Maningky M, Helder MN, et al. Virtual and traditional surgical planning in orthognathic surgery - systematic review and meta-analysis. Br J Oral Maxillofac Surg 2022;60:1184-91. [Crossref] [PubMed]
- Xu R, Ye N, Zhu S, et al. Comparison of the postoperative and follow-up accuracy of articulator model surgery and virtual surgical planning in skeletal class III patients. Br J Oral Maxillofac Surg 2020;58:933-9. [Crossref] [PubMed]
- Ying X, Tian K, Zhang K, et al. Accuracy of virtual surgical planning in segmental osteotomy in combination with bimaxillary orthognathic surgery with surgery first approach. BMC Oral Health 2021;21:529. [Crossref] [PubMed]
- Schneider D, Kämmerer PW, Hennig M, et al. Customized virtual surgical planning in bimaxillary orthognathic surgery: a prospective randomized trial. Clin Oral Investig 2019;23:3115-22. [Crossref] [PubMed]
Cite this article as: Pham SE, Gheibi Dehnashi N, Pearl CB, Dallaire-Giroux C, Arribas AR. Surgery first orthognathic approach: a case series of 3D planning and pre-bent plates in patients with single- and double-jaw surgeries. Front Oral Maxillofac Med 2024;6:33.


