
Orthopedic treatment of Class II malocclusion with mandibular deficiency: a clinical practice review
Introduction
Prevalence of Class II malocclusion
The prevalence of Class II malocclusion in North America is 24% (1). For communities of Northern European descent, the prevalence of Class II malocclusion could be as high as 30–40% (2,3). It has been shown that 8–10% of the population have an excess overjet more than six millimeters.
Diagnosis of Class II malocclusion
A proper diagnosis of the underlying cause of a malocclusion is essential to selecting an appropriate modality for treatment. McNamara suggested the evaluation of Class II problems in three planes of space (4).
Anteroposterior problems
The majority of Class II patients present with a convex facial profile. An important guide is the nasolabial angle which should be 102°±8° for both males and females (4). A more acute nasolabial angle signifies protrusion of the maxillary incisors. A lateral cephalometric radiograph may be used to evaluate the anteroposterior position of the maxilla, using the angle sella-nasion-A point of maxilla (SNA) (5,6) or angle from nasion perpendicular to point A (4). The position of the upper incisors relative to the maxilla can be evaluated from the facial surface of the upper incisor to a vertical line drawn perpendicular to the Frankfort horizontal plane extending through the A point and is ideally 4–6 mm (4,7). The lower incisor position may be determined by measuring the distance from the tip of the lower incisor to the A point-pogonion line (8,9). The position of the mandible relative to the cranial base may be determined by the angle sella-nasion-B point of mandible (SNB), or measurements from pogonion to nasion perpendicular (5,6).
Vertical problems
The vertical skeletal dimension provides information on the growth direction of the maxilla and the mandible (9,10). A decrease in vertical dimension signifies an upward and forward growth of the mandible. Conversely, an increase in vertical dimension may indicate a downward and backward growth of the mandible. A patient with mandibular retrognathia in combination with a decreased lower face height usually also has a hyperactive mentalis muscle; poorly defined chin projection, resulting in a tendency towards a malocclusion with deep overbite (11).
Transverse problems
The transverse relationship between the maxilla and the mandible may be assessed with a set of dental casts, digital intra-oral scans, or on a posterior-anterior cephalogram. Tollaro et al. have shown that Class II malocclusion with a normal buccal relationship can have an underlying transverse discrepancy of 3–5 mm (12). This becomes apparent when the patient was asked to posture the mandible forward to a Class I canine and molar relationships. Studies by Baccetti et al. (13) and Bishara et al. (14) indicated that this transverse discrepancy needs to be dealt with. Spillane and McNamara (15) recommended maxillary expansion to correct the maxillary transverse deficiency at a young age.
Treatment of Class II malocclusions
Non-growing patients
Treatment options for non-growing Class II patients include extractions, camouflage orthodontic tooth movement or orthognathic surgery. In moderate Class II malocclusions with minimal crowding, clinicians could attempt the maxillary molar distalization. It has been shown that 2 to 2.5 mm of maxillary molar distalization may be possible in adult patients without using skeletal anchorage devices (16). Class II patients with a severe anteroposterior skeletal discrepancy are best treated with orthognathic surgery at a later age to improve the facial profile.
Growing patients
In patients with growth remaining, clinicians can harness growth by performing growth modification during the peak pubertal growth spurt (17). This accelerated growth usually occurs around age 13.9±1.0 years in males and age 11.7±1.0 years in females. Functional appliances may be used to restrain maxillary growth or stimulate mandibular growth in patients with mild to moderate skeletal discrepancies. Extractions of permanent teeth may still be necessary in patients with poor growth potential or severely crowded dentition.
Treatment of Class II malocclusions with functional appliances
Functional appliances were popularized by the Andreason activator in Europe in the 1930’s (18,19). At that time, clinicians believed that these appliances forced the mandible forward to stimulate growth. Functional appliances may be divided into two general groups: removable and fixed. Removable appliances are worn by patients and may be removed when eating or brushing teeth to maintain oral hygiene. In patients who are not compliant, condylar growth adaptation may never reach the required threshold. Consequently, the treatment time could be longer and dependent on patient compliance. On the other hand, fixed functional appliances are not removable, and exert their effects on the dentition 24 hours a day. Patient compliance is usually not required other than maintaining good oral hygiene (20). With the advent of dental technology, modern removable appliances such as Invisalign® with mandibular advancement (MA) may prove to be more acceptable to patients (21). With better patient cooperation, the average treatment time may be similar to fixed functional appliances. This clinical practice review is unique in that it compares and contrasts a well-known fixed functional appliance such as the Herbst, with a relatively novel clear aligner appliance, Invisalign® with MA.
Knowledge gap and objective
There have been numerous systematic reviews on different modalities of Class II treatment, as well as mechanisms of action of various orthodontic appliances for Class II correction. These include Class II elastics, functional appliances like the Twin Block, Bionator and Herbst appliance. However, there are very few reviews that compare the treatment effects and treatment outcomes of different appliances. The effects and treatment outcomes of the Herbst appliance have been well documented by Pancherz and others. However, there has been very little published about the novel Invisalign® with MA appliance which was first launched in 2017. A comparison between a well established orthodontic appliance with a novel appliance that purports to have similar treatment effects, would be helpful to the clinician in the decision as to selecting an appropriate appliance for their patients’ malocclusion.
This clinical practice review is written to present the literature background of contemporary treatment of Class II malocclusion with mandibular deficiency using a fixed Herbst functional appliance and a removable Invisalign® with MA clear aligner functional appliance. Both of these appliances sequentially advance the mandible into a forward position for Class II correction. This review is illustrated with a clinical case treated with each type of functional appliance, as examples to demonstrate mechanism of action and treatment outcomes. An attempt is made in the discussion to compare the treatment effects of these two appliances and the overall treatment time.
The Herbst functional appliance
Background of the Herbst appliance
Emil Herbst attempted to posture the mandible forward in the early 1900’s by using an inclined plane (22). This fixed ‘bite jumping’ appliance used bilateral telescope arms attached to orthodontic bands of the lower first premolars and upper first molars to keep the mandibular in a forward position, thus changing mandibular jaw and muscle function (22). The Herbst appliance was used to treat patients with Class II malocclusions accompanied by a retrognathic mandible; as well as other patients with temporomandibular joint (TMJ) issues, mandibular ramus fractures and condylectomies (23).
In the 70’s, Hans Pancherz repopularized the Herbst appliance as one with potential to stimulate growth of the mandible (24). The Herbst design by Pancherz utilized custom-made orthodontic bands. However, orthodontists who used pre-formed orthodontic bands found frequent breakage due to heavy occlusal forces As a result, variations of the Herbst appliance were developed, including the use of cobalt chromium cast splints for better fit (25-27). Subsequently, McNamara and Howe introduced the removable acrylic splint Herbst appliances with occlusal coverage for posterior teeth in 1988 (28). The bonded appliance proved to be too difficult to remove and increased the risk of enamel decalcification. Another variation, the crowned Herbst appliance, was proposed by Langford in the 1990’s (29). This new Herbst design remains the most popular means of retaining the appliance today. However, the stainless steel crowns have drawbacks in that they tend to open the occlusion, cannot be adapted closely to the teeth, and interfere with mastication. They can also encroach on the gingiva, and are frequently difficult to remove (30).
Indications for Herbst appliance therapy
The Herbst appliance is indicated as a growth modification appliance for treatment of Class II malocclusion due to mandibular retrognathia. This appliance can sometimes be used in non-growing patients due to its dentoalveolar effects such as molar distalization. The disadvantage of using this appliance in adult patients is the risk of developing a dual bite (31). The Herbst appliance is now used in non-growing patients with mouth breathing habits, as well as non-cooperative patients in compliance of wearing elastics or removable functional appliances.
Contemporary design of the Herbst appliance
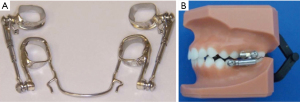
In 2001, Rogers (30,32) proposed the use of a reinforced banded Herbst appliance to prevent breakage of orthodontic bands and doubling the length of Herbst treatment for stability of MA. For stability, buccal archwire tubes were incorporated on the maxillary molar bands, and a larger 0.051-in lingual arch was used on the mandibular arch (Figure 1). A 0.051-in reinforcing wires were soldered to the distal occlusal margins of the maxillary and mandibular bands to reinforce the molar bands. In addition, a 0.025-in wires were soldered to the mesial occlusal margins of the mandibular and maxillary bands. The maxillary telescopes were secured to the maxillary pivots in the laboratory before trying on the Herbst by placing Ceka Bond (Specialty Appliances, Cumming, Georgia, USA) on the screw threads. The mandibular telescopes were secured after cementation. The advantage with this design is the ease of appliance removal. After removal of the mandibular screws, the bands were removed with a band-removing plier.
Timing of Herbst appliance therapy
Most literature agree that functional appliances should be used during the pubertal growth period (33). Successful treatment of Class II skeletal discrepancies have been reported in the late mixed dentition (34). A systematic review reported that if functional appliances were utilized during the peak growth period, the amount of additional mandibular growth was greater (35). The treatment timing also varied with the practice characteristics and training background of the operators (36). Studies have shown that patients with a half cusp molar relationship had better results with the appliance than patient with a full-cusp Class II molar relationships (37,38).
Treatment effects of Herbst appliance
Treatment with the Herbst appliance produces skeletal and dentoalveolar changes. The appliance postures the mandible forward and anchors on the maxilla, resulting in skeletal changes in both the maxilla and mandible. In addition, the appliance was worn by the patient full time resulting in distal movement of the upper dentition and mesial movement of the lower dentitions.
Skeletal effects
- Maxilla: the Herbst appliance has a restraining effect on maxillary growth similar to a headgear (38,39). Studies have shown that growth of the maxilla in patients treated with the Herbst appliance is less than the control groups. The total size of the maxilla was not affected by treatment. The palatal and occlusal planes rotated clockwise (39,40).
- Mandible: during a 6–8-month treatment interval, the Herbst appliance has been shown to increase mandibular length 1.3 to 3.5 mm compared to untreated controls (38-41). This was attributed to an increase in the sagittal condylar growth (42). Conversely, Chen et al. (43) reported in a systematic review that there is no difference in the horizontal or vertical direction of mandibular growth. In contradiction to this, Cozza et al. (35) found two-thirds of the samples reported a clinically significant supplementary increase in total mandibular length greater than 2 mm compared to controls.
- Temporomandibular region: the response of the temporomandibular joint to anterior positioning of the mandible remains controversial. A few investigators believe that the main effect of functional appliance therapy is an increase in condylar growth. Other investigators feel that the glenoid fossa remodels to accommodate the forward positioning of the mandible in order to keep the condyle concentric in the fossa (44,45).
Dental effects
- Maxillary dentition: significant changes in the maxillary dentition include distal and intrusive movements of the maxillary dentition such as in the case of a high-pull headgear effect (37,46).
- Mandibular dentition: in general, most investigators agreed that there is proclination of the mandibular incisors with the fixed Herbst treatment (38-41). However, the lower incisor proclination is reversed 60–80% during the post-Herbst phase of the treatment (45).
The Invisalign® with MA appliance
Background of Invisalign® with MA clear aligner appliance
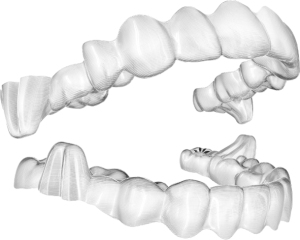
In 1945, Kesling first proposed moving teeth with a series of clear vacuum formed plastic appliances (47). Individual teeth had to be reset by hand and for each minor tooth movement, a separate thermoformed plastic appliance would be made. Eventually a series of these appliances would then align teeth. However, this method was too labor intensive to correct entire malocclusions. With the advent of new technology such as 3D printing with stereolithography and software development, clear aligners as an orthodontic appliance were launched in 1999 by a company called Align Technology Inc. (Tempe, AZ, USA). Initially, it was a simple orthodontic appliance that was capable of minor tooth movements with interproximal reduction to resolve crowding. Since then, clear aligner technology has evolved significantly to allow us to correct complex malocclusions. In 2017, Align Technology launched a new orthodontic appliance, a clear aligner with appliance with buccal extensions called precision wings (48) (Figure 2). These buccal extensions on both the upper and lower aligner are designed to posture the mandible forward in occlusion, simulating the mechanism of action of functional appliances for Class II skeletal correction. A series of aligners with precision wings would be worn and changed every 7 days. In addition to the antero-posterior correction that would take place over time, levelling and aligning would also occur simultaneously, presumably resulting in a more efficient treatment.
Indications for Invisalign® MA appliance therapy
Invisalign MA is indicated for Class II, retrognathic, growing patients where growth modification to address a Class II skeletal pattern, or a retrognathic, convex profile is desired. While other functional appliances have been shown to procline the lower incisors in treatment, the MA appliance has demonstrated excellent vertical and inclination control of the lower incisors (49). Therefore, where the lower incisors are already proclined in an attempt at dental compensation, but growth modification is the treatment of choice, one may consider the MA appliance for its ability to control the lower incisor position while posturing the mandible forward.
Timing of Invisalign® MA appliance therapy
The recommended age range for treatment with the MA appliance would be between age 11–16 years during the pubertal growth spurt. In mixed dentition patients age 10 and younger, mobile or exfoliated primary molars would preclude the placement of the precision wings. One critical requirement for Invisalign® MA is the presence of posterior teeth in all 4 quadrants whether the patient is in mixed or permanent dentition to allow for the placement of the precision wings. In patients older than 16 years old, there may be limited growth potential.
Treatment protocol of the Invisalign® MA appliance
The Invisalign® MA appliance consists of a series of clear aligners with buccal extensions called precision wings. In certain circumstances, there may be a pre-advancement phase of aligners before the precision wings are placed on the appliance. A pre-advancement phase would be required if any one of the following situations exist. If the overbite is deeper than 8 mm, there will be a pre-advancement phase consisting of aligners without precision wings to level the curve of Spee and decrease the overbite until it is less than 8 mm. If a posterior crossbite exists, then the maxillary arch will be expanded first before the precision wings are placed to advance the mandible. In Class II division 2 malocclusions, there will be a pre-advancement phase to align the maxillary incisors and increase the overjet to 2 mm before the first advancement of 2 mm. Finally, if the maxillary first molars are rotated more than 20 degrees, then the rotations will be corrected prior to placement of the precision wings (48).
In the advancement phase, the mandible is advanced sequentially 2 mm every 8 stages or 8 weeks, until the incisors are in an edge-to-edge position. The mandible is then held in the edge-to-edge position until the end of the advancement phase. The aligners are changed every 7 days. There is simultaneous tooth movement such as alignment and levelling of the curve of Spee that occurs during this phase (50). Since interproximal reduction is not permitted during the advancement phase, any crowding would be resolved through a combination of expansion and incisor proclination. Vertical elastics may be prescribed for night time wear to keep the aligners engaged in the forward position while sleeping. At the end of the advancement phase, there are 4 passive aligners to be worn while waiting for the additional aligners for the second phase. In the second phase, clear aligners without the precision wings are fabricated to complete any levelling and alignment, as well as detailing and finishing. If there was lower incisor crowding in the initial malocclusion then alignment may have resulted in lower incisor proclination. Interproximal reduction may be prescribed in the second phase to upright and retrocline the lower incisors to a more acceptable inclination. Additionally, Class II elastics are usually worn to maintain the advanced position of the mandible. If the Class II buccal relationship was not completely corrected to Class I during the advancement phase, upper molar distalization or an elastic simulation jump may be incorporated into the digital software plan to complete the correction to Class I.
Treatment effects of Invisalign® MA appliance therapy
Since the Invisalign® MA appliance was launched in 2017, and orthodontic treatment takes several years, there are only few studies on the efficacy and treatment effects for this appliance. In a comparison between Twin Block functional appliance and the MA appliance by Blackham (49) it was found that the MA appliance worked similar to the Twin Block in reducing the overjet, decreasing the angle A point-nasion-B point (ANB) and Wits measurement, and increasing SNB, skeletal and soft tissue convexity. The MA appliance offered excellent vertical control with little to no change in the mandibular plane angle. While the lower incisors tended to procline and erupt with the Twin Block appliance, with the MA appliance, the lower incisors were held in the same vertical plane due to continuous intrusion programmed into the aligners. It also maintained the inclination of the lower incisors very well.
A different study comparing Twin Block patients with Invisalign® MA patients also showed that both appliances were effective in correcting skeletal Class II malocclusions due to mandibular retrusion with similar treatment effects (51). Both groups offered excellent vertical control while there was more dental compensation of the upper incisors in the Twin Block group. A prospective study comparing pre-pubertal and pubertal patients showed that Invisalign® MA was effective in skeletal Class II growing patients with primarily dentoalveolar changes in the pre-pubertal group and dental skeletal changes in the pubertal group (52). Another study by Glaser et al. similarly found statistically significant changes in SNB, ANB, Wits appraisal and facial convexity contributing to the Class II correction. There was an average increase in mandibular length of 3.59 mm. Overbite and overjet also reduced favorably. The MA appliance offered excellent vertical control with no statistically significant changes in SN-MP, Frankfort mandibular plane angle (FMA), interincisal angle or incisor mandibular plane angle (IMPA) (53).
In a master’s thesis comparing Class II patients treated with the Herbst and the Invisalign® MA appliance using the Pancherz’s methodology (54) it was found that in the advancement phase with Invisalign® MA, both the overjet and molar relationship correction was achieved primarily by skeletal change with minor dental contribution. The lower incisors were retracted rather than proclined. The mandible moved forward by 4 mm which was both statistically and clinically significant. The overall treatment time with the MA appliance was 4 months shorter when compared with the Herbst appliance.
Case presentation: the Herbst appliance
Diagnosis and etiology
A 12-years 5 months-old male patient (L.W.) presented with a chief concern of “excess overbite”. The patient’s main complaints were excessive daytime sleepiness and fatigue. Clinical and radiographical examination revealed a convex facial profile with maxillary and mandibular retrognathism (Figure 3). Intra oral examination revealed a Class II division 1 malocclusion with mild dental spacing, maxillary transverse deficiency, excess overjet and overbite (Figure 4). Cephalometric and facial analysis indicated that patient had a hypodivergent growth pattern with a convex profile and a shallow mentolabial fold, small lip protrusion and normal nasolabial angle (Table 1, Figures 5,6). The skeletal maturation was determined to be pre-peak pubertal growth around cervical vertebral maturation (CVM) 3.

Table 1
| Variable | Pretreatment | Posttreatment | Average |
|---|---|---|---|
| SNA (°) | 78 | 78 | 82 |
| SNB (°) | 76 | 77 | 80 |
| ANB (°) | 2 | 1 | 2 |
| IMPA (°) | 104 | 94 | 90 |
| FMA (°) | 15 | 17 | 25 |
| 1/SN (°) | 94 | 93 | 104 |
| Wits (mm) | 2.5 | 1 | 1.1 |
| LFH/TFH (%) | 52 | 53 | 55 |
| Distance of upper lip to esthetic plane (mm) | −7 | −6 | 3 |
| Distance lower lip to esthetic plane (mm) | −7 | −7 | 1 |
SNA, angle sella-nasion-A point of maxilla; SNB, angle sella-nasion-B point of mandible; ANB, angle A point-nasion-B point; IMPA, incisor mandibular plane angle; FMA, Frankfort mandibular plane angle; 1/SN, upper incisor to sella nasion plane angle; Wits, Wits appraisal; LFH/TFH, ratio of lower face height to total face height.
Treatment objectives
The treatment objectives for this patient included orthodontic treatment to correct maxillary transverse discrepancy, eliminate dental crowding, create, establish overbite and overjet for proper function, and improve soft tissue profile.
Treatment alternatives
Comprehensive orthodontic treatment with full fixed appliance with rapid palatal expansion appliance to correct maxillary transverse deficiency and Class II elastics to improve overjet and molar relationship. Patient was judged to have favorable forward and upward mandibular growth due to adequate corpus and ramal length together with hypodivergent growth pattern. The use of a Herbst appliance to facilitate correction of overjet and overbite was offered to patient to reduce the amount of patient compliance and reduce treatment time. After discussing the treatment alternatives with the patient and explaining the benefits and expected outcomes, patient elected to have the Herbst appliance followed by fixed appliance.
Treatment progress
The patient was treated with a reinforced banded Herbst appliance together with a rapid maxillary expansion appliance as described earlier (Figures 7,8). Stepwise advancement of the mandible (2 mm/2 months) was performed until the mandible was advanced to an edge to edge incisal relationship. The total orthopedic treatment time was 12 months. This was immediately followed by comprehensive orthodontic treatment with fixed appliances to correct the remaining overjet and overbite. After 22 months of active treatment, the appliance was debonded. A clear retainer was placed in both the maxillary and mandibular arches. The final results were shown in Figures 9,10.

Treatment results
The occlusion was finished in an ideal Class I canine and molar relationship. The overbite and overjet was improved. The patient was satisfied with the esthetic outcome. The post treatment panoramic radiograph indicated well-aligned roots with minimal root resorption (Figure 11). Superimposition of the pretreatment and post treatment lateral cephalograms (Figure 12) revealed downward movement of the maxilla, restraint of forward maxillary growth and good forward and upward growth of the mandible. The maxillary incisors were maintained, and the mandibular incisors were slightly proclined (Figure 13). The occlusion and facial esthetics were stable 2 years after removal of appliances.
Case presentation: Invisalign® MA appliance
Diagnosis and etiology
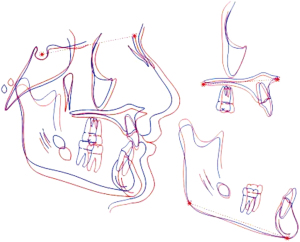
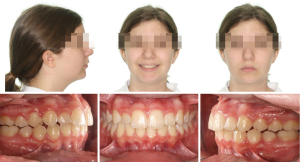
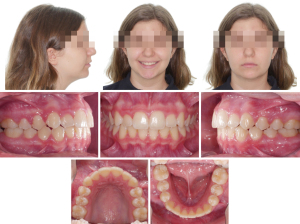
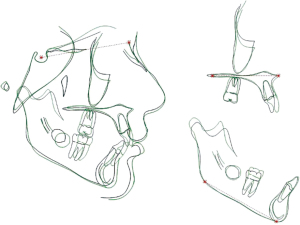
A 12-years 1 month-old female presented with a main concern of a “retruded facial profile”. Her mother recently had MA orthognathic surgery for a severe skeletal Class II malocclusion. The patient presented with a convex profile with decreased lower face height, mandibular retrognathia, decreased chin-throat length and prominent labio-mental fold. Intra-orally, the patient presented with a Class II malocclusion with moderate crowding in the upper arch and buccally erupted canines. The maxillary lateral incisors had erupted palatally. There was minor crowding in the lower arch (Figures 14,15). Cephalometric analysis revealed a severe Class II skeletal pattern with ANB of +6.3 degrees and mandibular retrognathia (Table 2). She had a hypodivergent growth pattern with increased mandibular plane angle. The skeletal maturation was determined to be CVM 3 (Figure 16).

Table 2
| Variable | Pretreatment | Posttreatment | Average |
|---|---|---|---|
| SNA (°) | 79.6 | 77.6 | 82.0 |
| SNB (°) | 73.3 | 74.5 | 80.0 |
| ANB (°) | 6.3 | 3.2 | 2.0 |
| IMPA (°) | 96.8 | 96.3 | 90.0 |
| FMA (°) | 30.6 | 29.4 | 25.0 |
| 1/SN (°) | 95.0 | 99.3 | 104 |
| Wits (mm) | 2.1 | −3.4 | 1.1 |
| LFH/TFH (%) | 50 | 51.5 | 55 |
| Distance of upper lip to esthetic plane (mm) | −7 | −6 | 3 |
| Distance lower lip to esthetic plane (mm) | −10 | −9 | 1 |
MA, mandibular advancement; SNA, angle sella-nasion-A point of maxilla; SNB, angle sella-nasion-B point of mandible; ANB, angle A point-nasion-B point; IMPA, incisor mandibular plane angle; FMA, Frankfort mandibular plane angle; 1/SN, upper incisor to sella nasion plane angle; Wits, Wits appraisal; LFH/TFH, ratio of lower face height to total face height.
Treatment objectives
The treatment objectives for this patient are to improve the soft tissue facial profile, correct the Class II skeletal discrepancy, align upper and lower dental arches to finish with a Class I canine and molar relationship and normal overbite and overjet.
Treatment alternatives
Treatment alternatives discussed with the patient were Twin Block functional appliances for skeletal correction, followed by fixed edgewise appliances, or extractions of maxillary first premolars which would allow us to resolve crowding in the upper arch, but likely would be detrimental to the facial profile. After discussion of the advantages and disadvantages of each appliance and treatment approach, the patient and her mother chose treatment with MA appliance.
Treatment progress
Invisalign® with MA with precision wings were placed (Figure 17). The mandible was advanced 2 mm every 8 stages (2 months) until the incisors were in and edge-to-edge position. Simultaneous alignment and levelling in both upper and lower dental arches were performed together with the antero-posterior correction. The aligners were changed every 7 days. There were 42 aligners in the advancement phase. The advancement phase was completed in 10 months. The patient was held in passive aligners while waiting for additional aligners for the second phase of treatment to arrive. At the end of the advancement phase, the molar relationship had been corrected to Class I. The overbite and overjet were within normal limits. The canine relationship was a mild Class II, there was some minor alignment issues remaining and mild midline discrepancy (Figure 18). A progress cephalometric radiograph (Figure 19) was taken and superimposition of the lateral cephalograms (Figure 20) to assess any skeletal and dental changes that occurred.

There were 16 aligners in the additional aligner phase. Precision cuts for Class II elastics were designed to complete the correction to Class I. The patient wore 1/4 inch 4 oz elastics full time. Interproximal reduction of 0.2 mm was performed in the lower anterior segment to upright the lower incisors to a normal inclination. Total treatment time was 20 months. The patient was retained with clear vacuum formed retainers in both upper and lower dental arches.
Treatment results
The patient’s facial profile improved significantly with an increase in chin projection and lower face height. Both upper and lower dental arches were well aligned with coincident dental midlines. The buccal relationship was corrected to Class I canine and Class I molar (Figure 21). Cephalometric measurements and superimpositions show a decrease in ANB, increase in SNB and forward movement of the mandible. The upper incisors were proclined, while the lower incisor inclination was maintained. Overbite and overjet were corrected to normal limits (Figures 22,23).
Discussion
Both the fixed Herbst appliance and the removable MA appliance can achieve satisfactory correction of patients with Class II malocclusions and mandibular deficiency. The use of a fixed Herbst appliance has the advantage of minimizing compliance from the patient. On the other hand, the patient must exercise good oral hygiene. The use of reinforced molar bands minimizes breakage of the appliance during treatment. Overcorrection of the MA and increase in orthopedic treatment time allows stability of MA during finishing of orthodontic treatment. However, proclination of mandibular incisors remain a concern to the clinicians, especially in cases with already proclined lower incisors.
As for the MA appliance, it was found that the average treatment times were similar to those treated using the Twin Block appliances (49), but on average less than that of the Herbst appliance (54). This is likely attributed to the levelling and alignment that occurs simultaneously with the antero-posterior correction. Unlike the Herbst appliance where the end point of the advancement phase was an edge-to-edge occlusion, for the MA patients, the occlusion was corrected to ideal overbite and overjet at the end of the advancement phase. Statistically, significant changes were found in the SNB, ANB, Wits appraisal and facial convexity which contributed to the Class II correction. There was an average increase in mandibular length of 3.59 mm. Overbite and overjet were also reduced favorably. The MA appliance offered excellent vertical control especially with lower molar position and lower incisors, with no statistically significant changes in SN-MP, FMA, interincisal angle or IMPA (53). Multiple studies corroborate these findings and mechanism of action of the MA appliance (49-54).
Some of the limitations of this review is that while the Herbst appliance has been extensively studied with multiple literature references, the MA appliance was only launched in 2017 globally and thus there are few studies published on its treatment effects. Most of the studies, however, are very current, having been published within the last 3 years. These studies, while few in number, corroborate the treatment effects and outcomes achieved with this novel clear aligner functional appliance.
While this clinical practice review demonstrated the treatment effects of one case treated with each appliance, the treatment effects seen in the illustration were representative of the treatment changes seen in studies performed on the Herbst and Invisalign® MA appliance. Since Invisalign® MA is still a relatively new functional appliance, it is recommended that further studies be done on its treatment effects, as well as comparison to other commonly used Class II correctors to compare its treatment outcomes and effects with the current standards in orthodontic practice. Understanding the mechanisms of action, similarities and differences in treatment outcomes with each individual appliance may assist clinicians in selecting the appropriate orthodontic functional appliance for Class II treatment.
Conclusions
Both the fixed Herbst appliance and the removable MA appliance can achieve satisfactory correction of patients with Class II malocclusions and mandibular deficiency. The average treatment time with the removable MA appliance may be shorter due to leveling and alignment that can be performed at the same time with anteroposterior correction. Over-correction of overjet and molar relationship is not necessary with the removable MA appliance. Vertical control may be better with the use of aligners in Class II cases with a hyperdivergent mandibular growth pattern. Oral hygiene may be better with removable rather than fixed appliance. On the other hand, if patient compliance is not forthcoming, the use of fixed appliance such as the reinforced banded Herbst design may be a better choice.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Chung H. Kau) for the series “Managing Craniofacial and Dentofacial Disorders—Simplified Solutions for Difficult Situations” published in Frontiers of Oral and Maxillofacial Medicine. The article has undergone external peer review.
Peer Review File: Available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-69/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure forms (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-69/coif). The series “Managing Craniofacial and Dentofacial Disorders—Simplified Solutions for Difficult Situations” was commissioned by the editorial office without any funding or sponsorship. S.K.T. reports that she is a member of the Clinical Advisory Board North America for Align Technology Inc., the manufacturer of the Invisalign with Mandibular Advancement appliance and is paid an annual stipend as a board member. S.K.T. is a member of Align Tech Global faculty, lectures for Align Tech globally and receives honoraria for speaking at Align sponsored conferences. Align Technology Inc. will sponsor travel to an Align organized event where S.K.T. is lecturing. S.K.T. does not receive stock options, but privately owns some stock in Align Technology Inc. (ALGN). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patients for publication of their images. For patients under 18 years informed consents were obtained from their parents. Copies of the written consent are available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- McLain JB, Proffitt WR. Oral health status in the United States: prevalence of malocclusion. J Dent Educ 1985;49:386-97. [Crossref] [PubMed]
- Bilgic F, Gelgor IE, Celebi AA. Malocclusion prevalence and orthodontic treatment need in central Anatolian adolescents compared to European and other nations' adolescents. Dental Press J Orthod 2015;20:75-81. [Crossref] [PubMed]
- Josefsson E, Bjerklin K, Lindsten R. Malocclusion frequency in Swedish and immigrant adolescents--influence of origin on orthodontic treatment need. Eur J Orthod 2007;29:79-87. [Crossref] [PubMed]
- McNamara JA Jr. A method of cephalometric evaluation. Am J Orthod 1984;86:449-69. [Crossref] [PubMed]
- Riedel RA. The relationship of maxillary structures to cranium in malocclusion and normal occlusion. Angle Orthod 1952;22:142-45.
- Steiner CC. Cephalometrics for you and me. Am J Orthod 1953;39:729-55. [Crossref]
- McNamara JA Jr, Ellis E 3rd. Cephalometric analysis of untreated adults with ideal facial and occlusal relationships. Int J Adult Orthodon Orthognath Surg 1988;3:221-31. [PubMed]
- Ricketts RM. The influence of orthodontic treatment on facial growth and development. Angle Orthod 1960;30:103-33.
- Schudy FF. Vertical growth versus anteroposterior growth as related to function and treatment. Angle Orthod 1964;34:75-93.
- Schudy FF. The Rotation Of The Mandible Resulting From Growth: Its Implications In Orthodontic Treatment. Angle Orthod 1965;35:36-50. [PubMed]
- McNamara JA Jr. Components of class II malocclusion in children 8-10 years of age. Angle Orthod 1981;51:177-202. [PubMed]
- Tollaro I, Baccetti T, Franchi L, et al. Role of posterior transverse interarch discrepancy in Class II, Division 1 malocclusion during the mixed dentition phase. Am J Orthod Dentofacial Orthop 1996;110:417-22. [Crossref] [PubMed]
- Baccetti T, Franchi L, McNamara JA Jr, et al. Early dentofacial features of Class II malocclusion: a longitudinal study from the deciduous through the mixed dentition. Am J Orthod Dentofacial Orthop 1997;111:502-9. [Crossref] [PubMed]
- Bishara SE, Hoppens BJ, Jakobsen JR, et al. Changes in the molar relationship between the deciduous and permanent dentitions: a longitudinal study. Am J Orthod Dentofacial Orthop 1988;93:19-28. [Crossref] [PubMed]
- Spillane LM, McNamara JA Jr. Maxillary adaptation to expansion in the mixed dentition. Semin Orthod 1995;1:176-87. [Crossref] [PubMed]
- Ravera S, Castroflorio T, Garino F, et al. Maxillary molar distalization with aligners in adult patients: a multicenter retrospective study. Prog Orthod 2016;17:12. [Crossref] [PubMed]
- Baccetti T, Franchi L, Toth LR, et al. Treatment timing for Twin-block therapy. Am J Orthod Dentofacial Orthop 2000;118:159-70. [Crossref] [PubMed]
- Civen OI. An historical review of the progress of orthodontics from 1840-1940. Am J Orthod Oral Surg 1945;31:203-13. [Crossref]
- Baccaglione G, Rota E, Ferrari M, et al. Second Class Functional Treatment: Andreasen Activator vs Twin Block. Int J Clin Pediatr Dent 2020;13:144-9. [Crossref] [PubMed]
- Pancherz H. Treatment of class II malocclusions by jumping the bite with the Herbst appliance. A cephalometric investigation. Am J Orthod 1979;76:423-42. [Crossref] [PubMed]
- ALIGN. Align Technology Announces New Teen Solution With Introduction of Invisalign Teen With Mandibular Advancement. 2017. Available online: https://investor.aligntech.com/news-releases/news-release-details/align-technology-announces-new-teen-solution-introduction
- Hanks SD. Trying to get out of the 20th century: a partial translation of Emil Herbst’s 1910 text. World Journal of Orthodontics 2000;1.
- Herbst E. Dreissigjahrige Erfahrungen mit demRetentionsscharnier. Zahnärztl Rundschau 1934;43:1515-24, 1563-68, 1611-16, 1934.
- Pancherz H. The Herbst appliance--its biologic effects and clinical use. Am J Orthod 1985;87:1-20. [Crossref] [PubMed]
- Dischinger T. Edgewise Herbst Appliance. J Clin Orthod 1995;29:738-42. [PubMed]
- Mayes JH. Improving appliance efficiency with the Cantilever Herbst. A new answer to old problems. Clin Impressions 1994;3:2-5.
- Moro A, Janson G, de Freitas MR, et al. Class II correction with the Cantilever Bite Jumper. Angle Orthod 2009;79:221-9. [Crossref] [PubMed]
- McNamara JA, Howe RP. Clinical management of the acrylic splint Herbst appliance. Am J Orthod Dentofacial Orthop 1988;94:142-9. [Crossref] [PubMed]
- Langford NM Jr. Updating fabrication of the Herbst appliance. J Clin Orthod 1982;16:173-4. [PubMed]
- Rogers MB. The banded Herbst appliance. J Clin Orthod 2001;35:494-9. [PubMed]
- Egermark-Eriksson I, Carlsson GE, Ingervall B. Function and dysfunction of the masticatory system in individuals with dual bite. Eur J Orthod 1979;1:107-17. [Crossref] [PubMed]
- Tomblyn T, Rogers M, Andrews L 2nd, et al. Cephalometric study of Class II Division 1 patients treated with an extended-duration, reinforced, banded Herbst appliance followed by fixed appliances. Am J Orthod Dentofacial Orthop 2016;150:818-30. [Crossref] [PubMed]
- Pancherz H, Hägg U. Dentofacial orthopedics in relation to somatic maturation. An analysis of 70 consecutive cases treated with the Herbst appliance. Am J Orthod 1985;88:273-87. [Crossref] [PubMed]
- Pancherz H. The mechanism of Class II correction in Herbst appliance treatment. A cephalometric investigation. Am J Orthod 1982;82:104-13. [Crossref] [PubMed]
- Cozza P, Baccetti T, Franchi L, et al. Mandibular changes produced by functional appliances in Class II malocclusion: a systematic review. Am J Orthod Dentofacial Orthop 2006;129:599.e1-12; discussion e1-6. [Crossref] [PubMed]
- Yang EY, Kiyak HA. Orthodontic treatment timing: a survey of orthodontists. Am J Orthod Dentofacial Orthop 1998;113:96-103. [Crossref] [PubMed]
- Hansen K, Pancherz H. Long-term effects of Herbst treatment in relation to normal growth development: a cephalometric study. Eur J Orthod 1992;14:285-95. [Crossref] [PubMed]
- Pancherz H, Fackel U. The skeletofacial growth pattern pre- and post-dentofacial orthopaedics. A long-term study of Class II malocclusions treated with the Herbst appliance. Eur J Orthod 1990;12:209-18. [Crossref] [PubMed]
- Hägg U, Pancherz H. Dentofacial orthopaedics in relation to chronological age, growth period and skeletal development. An analysis of 72 male patients with Class II division 1 malocclusion treated with the Herbst appliance. Eur J Orthod 1988;10:169-76. [Crossref] [PubMed]
- Lai M, McNamara JA Jr. An evaluation of two-phase treatment with the Herbst appliance and preadjusted edgewise therapy. Semin Orthod 1998;4:46-58. [Crossref] [PubMed]
- McNamara JA Jr, Howe RP, Dischinger TG. A comparison of the Herbst and Fränkel appliances in the treatment of Class II malocclusion. Am J Orthod Dentofacial Orthop 1990;98:134-44. [Crossref] [PubMed]
- Pancherz H. Vertical dentofacial changes during Herbst appliance treatment. A cephalometric investigation. Swed Dent J Suppl 1982;15:189-96. [PubMed]
- Chen JY, Will LA, Niederman R. Analysis of efficacy of functional appliances on mandibular growth. Am J Orthod Dentofacial Orthop 2002;122:470-6. [Crossref] [PubMed]
- VanLaecken R, Martin CA, Dischinger T, et al. Treatment effects of the edgewise Herbst appliance: a cephalometric and tomographic investigation. Am J Orthod Dentofacial Orthop 2006;130:582-93. [Crossref] [PubMed]
- Wigal TG, Dischinger T, Martin C, et al. Stability of Class II treatment with an edgewise crowned Herbst appliance in the early mixed dentition: Skeletal and dental changes. Am J Orthod Dentofacial Orthop 2011;140:210-23. [Crossref] [PubMed]
- Pancherz H, Hansen K. Occlusal changes during and after Herbst treatment: a cephalometric investigation. Eur J Orthod 1986;8:215-28. [Crossref] [PubMed]
- Kesling HD. The philosophy of the tooth positioning appliance. Am J Orthod Oral Surg 1945;31:297-304. [Crossref]
- Tai S. Chapter 10. Class II Treatment, page 36. Clear Aligner Technique. Quintessence Publishing; 2018:166.
- Blackham SS. A study of short term skeletal, dental, and soft tissue effects of Class II malocclusions treated with Invisalign® with Mandibular advancement feature or Twin Block appliance compared with historical controls. Master’s Thesis 2020, University of British Columbia.
- Available online: https://learn.invisalign.com/videos/MA-DrTai-clinicalprotocols-bestpractice
- Caruso S, Nota A, Caruso S, et al. Mandibular advancement with clear aligners in the treatment of skeletal Class II. A retrospective controlled study. Eur J Paediatr Dent 2021;22:26-30. [PubMed]
- Ravera S, Castroflorio T, Galati F, et al. Short term dentoskeletal effects of mandibular advancement clear aligners in Class II growing patients. A prospective controlled study according to STROBE Guidelines. Eur J Paediatr Dent 2021;22:119-24. [PubMed]
- Glaser BJ, Tai SK, Blevins R, et al. Prospective multicenter investigation of Invisalign treatment with the mandibular-advancement feature: An interim report. J Clin Orthod 2022;56:458-63. [PubMed]
- Hosseini HR. A comparison of skeletal, dental changes in Class II patients treated with Invisalign® with Mandibular Advancement and Herbst appliance. Master’s Thesis 2022, University of British Columbia.
Cite this article as: Ngan P, Tai SK. Orthopedic treatment of Class II malocclusion with mandibular deficiency: a clinical practice review. Front Oral Maxillofac Med 2024;6:27.














