
Using zinc oxide-based temporary materials as contrast methods: a practical and simple approach for planning prosthetically driven sinus elevation
Introduction
Adequate communication between the restorative dentists and surgeon is necessary to ensure adequate preparation of the receptor site subsequent and implant placement (1-5). Radiographic templates combined with cone beam computerized tomography (CBCT) are valuable tools to visualize the relationship between the planned restoration with the bone and other important anatomical structures (6,7). Traditionally, surgical and radiographic templates used radiopaque materials to show the contours of the planned restoration in the tomographic exam. Temporary restorative materials, gutta percha, barium sulfate, radiopaque putty, radiopaque artificial teeth, lead foil, steel, and amalgam have been used successfully (8,9). However, some of these materials are relatively expensive, require specific equipment to be used, or can be hard to apply properly to recreate the desired contours of the proposed restorations (6-9). This article presents the use of zinc oxide-based restorative materials as a radiopaque medium to aid the planning and execution of a bilateral sinus elevation. This alternative is a feasible and straightforward option for the clinical situation where modern techniques such as guided surgery are not an option (5). This article was presented in accordance with the MDAR reporting checklist (available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-11/rc).
Technique
In the present brief report, no human experiments were conducted, therefore no ethics committee approval was necessary. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). As part of routine dental care, this patient gave consent to radiographic imaging and photography at The Ohio State University College of Dentistry and agreed to share the images for scholastic purposes.
- Make maxillary and mandibular preliminary impression using irreversible hydrocolloid (Geltrate; Dentsply Sirona, Charlotte, NC, USA) and fabricate preliminary casts using fast-setting type IV dental stone (Snap Stone; WhipMix Corp., Louisville, KY, USA).
- Articulate the maxillary and mandibular casts and create artificial teeth arrangements using the manufacture method of your preference.
- Make sure the artificial teeth arrangements have a channel in their long axes for radiographic reference; a cylindric laboratory carbide cutter (H79Q.11.040 HP Q Cutter Carbide; Brasseler USA, Savannah, GA, USA) can be used for this purpose. If possible, extend the artificial teeth arrangements posteriorly to ensure posterior occlusal contacts to stabilize the radiographic template intraorally during the CBCT procedure. If needed apply a small amount of cyanoacrylate resin (Gorilla super glue brush & nozzle; Gorilla Glue Co., Cincinnati, OH, USA) to fix the artificial teeth arrangements to the cast.
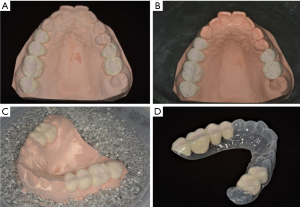
- Apply a thin coat of zinc oxide-based temporary cement (TempBond NE; Kerr Dental, Brea, CA, USA) to the surface of the artificial teeth arrangements and fill the channel of the artificial teeth with zinc oxide-based temporary filling material (Cavit temporary filling material; 3M ESPE, St Paul, MN, USA) (Figure 1A).
- Immerse the cast and artificial teeth arrangements in a rubber mixing bowl (Patterson Flex Mixing Bowl; Patterson Dental, Mendota, MN, USA) with lukewarm water to accelerate the setting of the zinc oxide-based restorative materials (Figure 1B). This step simplifies the separation of the artificial teeth arrangements from the casts at later stages since the bond between the teeth and the stone is decreased by water immersion.
- Using a pressure-molding device (Biostar Scan with LCD Display; Great Lakes Dental Technologies, Buffalo, NY, USA) create the external surface of the template using a thermoplastic polymer (Clear Splint Biocryl 1 mm/125 mm; Great Lakes Dental Technologies) (Figure 1C).
- Finish and polish the radiographic templates using laboratory carbide cutters and abrasive brushes (25525HP Fine Scotch Brite Brush: Patterson Dental) (Figure 1D). Make sure not to over trim the template material extending below the height of contour to ensure satisfactory mechanical retention of the artificial teeth arrangements within the template when removed from the cast.
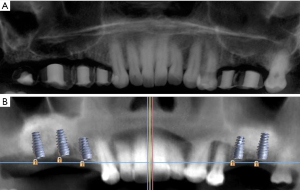
- Perform CBCT with the patient using the radiographic template (Figure 2A). The radiographic template can be used as a reference during surgery to estimate the amount of augmentation required for the subsequent rehabilitation (Figure 2B).
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-11/rc
Data Sharing Statement: Available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-11/dss
Peer Review File: Available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-11/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-11/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This brief report is not a research manuscript involving human experiments, hence ethical approval was not necessary. As part of routine dental care, this patient gave consent to radiographic imaging and photography at The Ohio State University College of Dentistry and agreed to share the images for scholastic purposes.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Engelman MJ, Sorensen JA, Moy P. Optimum placement of osseointegrated implants. J Prosthet Dent 1988;59:467-73. [Crossref] [PubMed]
- Steele J, Khan Z, Steiner M, et al. Stent-aided imaging for osseointegrated implants. Oral Surg Oral Med Oral Pathol 1990;70:243. [Crossref] [PubMed]
- Cho SW, Yang BE, Cheon KJ, et al. A Simple and Safe Approach for Maxillary Sinus Augmentation with the Advanced Surgical Guide. Int J Environ Res Public Health 2020;17:3785. [Crossref] [PubMed]
- Neidlinger J, Lilien BA, Kalant DC Sr. Surgical implant stent: a design modification and simplified fabrication technique. J Prosthet Dent 1993;69:70-2. [Crossref] [PubMed]
- Strbac GD, Giannis K, Schnappauf A, et al. Guided Lateral Sinus Lift Procedure Using 3-Dimensionally Printed Templates for a Safe Surgical Approach: A Proof-of-Concept Case Report. J Oral Maxillofac Surg 2020;78:1529-37. [Crossref] [PubMed]
- Zahran MH, Fenton A. A radiopaque implant template for partially edentulous patients. J Prosthet Dent 2010;103:390-2. [Crossref] [PubMed]
- Pesun IJ, Gardner FM. Fabrication of a guide for radiographic evaluation and surgical placement of implants. J Prosthet Dent 1995;73:548-52. [Crossref] [PubMed]
- Chong J, Seong WJ, Conrad HJ. Lead foil technique for partially edentulous radiographic guide. J Prosthet Dent 2012;108:268-70. [Crossref] [PubMed]
- Basten CH, Kois JC. The use of barium sulfate for implant templates. J Prosthet Dent 1996;76:451-4. [Crossref] [PubMed]
Cite this article as: Azpiazu-Flores FX, Lee DJ. Using zinc oxide-based temporary materials as contrast methods: a practical and simple approach for planning prosthetically driven sinus elevation. Front Oral Maxillofac Med 2024;6:24.

