
Antibiotic prophylaxis for animal inflicted maxillofacial injuries: a systematic review and meta-analysis
Highlight box
Key findings
• The use of antibiotic prophylaxis is not mandatory for all maxillofacial bite injuries.
What is known and what is new?
• Maxillofacial injuries inflicted by animals are usual worldwide.
• Bacterial resistance and risk of infection must be carefully considered before prescribing antibiotic prophylaxis.
What is the implication, and what should change now?
• Some protocols must be updated and further research is needed to confirm these findings. Antibiotic prophylaxis should not be mandatory in all bites in head and neck region. Special attention must be provided notably due to antibiotic resistance.
Introduction
An estimated 4.5 million dog bites occur across America each year (1). Bears, wild boars, snakes, leopards, crocodiles, and a variety of animals besides domestic ones have been reported to cause injuries. The number of attacks from wild animals is increasing and the main reason is human spread through wild areas (2). The social distancing measures during the pandemic significantly increased the number of attacks from domestic animals (3). Head and neck suffer more of these injuries because the maxillofacial region has a prominent anatomical position. It is estimated that 1% of all emergency room visits across the globe are due to animal bites (4). The overall range is hard to calculate due to the fact such a lot of attacks go unreported, however with this simple calculation it is possible to see the significance of animal attack management on the face. Human bites have to be additionally be a topic of research because the annual count is alarmingly growing (5,6).
Animal and human bites to the maxillofacial region are susceptible to contamination, making appropriate initial treatment crucial for preventing infections. The diverse range of bacteria found in these bites includes Streptococcus, Escherichia coli (E. coli), Pasteurella, Prevotella, Bacteroides, and others. While it is generally reasonable to use broad-spectrum antibiotic therapy to target both aerobic and anaerobic bacteria in most cases (7); there is no consensus within the literature regarding antibiotic prophylaxis, regardless of the animal species involved, type of wound, and other features (8-10). Although some authors contend that facial bite injuries exhibit a lower susceptibility to infection compared to injuries in other anatomical regions (6,10-12), it’s crucial to acknowledge the global apprehension regarding bacterial resistance and the overuse of antibiotics (13,14). This highlights the need for a balanced approach in determining the appropriateness of antibiotic prophylaxis in maxillofacial bite injuries, taking into consideration both the potential risks and benefits associated with their use.
The topic suffers from a dearth of recent articles, with a noticeable absence of a systematic review regarding animal bites. Therefore, the aim of this work is to systematically review the literature to answer whether antibiotic prophylaxis is obligatory in instances of animal and human maxillofacial bite injuries to prevent contamination of wounds. This query has to be discussed because of excessive bacterial resistance worldwide. In non-mandatory instances, antibiotic prophylaxis has to be avoided. We present this article in accordance with the PRISMA reporting checklist (15) (available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-18/rc).
Methods
Search strategy
A systematic literature search was conducted for records of antibiotic prophylaxis and animal or human maxillofacial bite injuries. The search was conducted within the PubMed, Web of Science (WS), Cochrane, Virtual Health Library (BVS), and Google Scholar (GS) databases. Databases were searched from inception until August 31, 2023. The following strategy was used: ((bite OR (bites and stings) OR (bites, human)) AND (face OR head OR neck) AND (antibiotic OR prophylaxis) NOT hand) in PubMed, WS, Cochrane, and BVS. Because the search algorithm is different, an adaptation of the strategy using Boolean operators, quotation marks, or signals + and - was performed on GS: (+bite[title] +face +antibiotic -hand +trial -“case report” -“systematic review” -meta-analysis -letters -notes -editorials). A manual reference list search of the included records was performed to identify additional records relevant to the study.
The authors intended to answer the following focused question according to the PICO acronym: Should patients who have been victims of maxillofacial bite injuries (P) undergo antibiotic prophylaxis (I) or is it not mandatory (C) to reduce the occurrence of wound infection (O)? This review is registered on PROSPERO under the number CRD 42022327242.
Two researchers (R.G. and Y.S.S.) independently screened the titles and abstracts of all records for relevance. Disagreements were solved by a third author (M.A.B.). Records without an abstract underwent a full-text check. Irrelevant records were excluded. After an initial selection on title and abstract, the full texts of relevant data sets were retrieved. Full-text records were screened for eligibility based on predetermined inclusion and exclusion criteria. The inclusion criteria were (I) original research reporting maxillofacial bite injuries; (II) studies focusing on antibiotic prophylaxis; (III) written in any language; and (IV) year of publication. Exclusion criteria were (I) reviews, case reports, conference abstracts, letters, notes, and editorials; (II) animal studies; (III) studies including <10 patients; (IV) topical antibiotic use; and (V) studies in which all patients have received antibiotic prophylaxis. No restriction was considered based on patient age, comorbidities, or other health conditions.
Data extraction
The following data was extracted from the included records: type of study, number of included patients, gender, mean age, types of attacks (animal or human), most commonly used antibiotic. The main outcome is the comparison of the number of wound infections in antibiotic and non-antibiotic prophylaxis for animal bites in the maxillofacial area.
Risk of bias across studies
Risk of bias across studies was assessed according Cochrane Risk of Bias Tool (RoB1). RStudio® (RStudio, GNU General Public License) was used to perform Egger’s regression test and considered significant only with a 95% confidence interval (CI). The Review Manager Software [RevMan 5.4 (Computer Program), Copenhagen: The Nordic Cochrane Centre, 2014] was used to rate all studies for quality of evidence. The queries of the included studies are briefly explained in Figure 1.
Statistical analysis
The effect measure was assessed using risk difference (RD) via RevMan 5.4 and considered significant at P<0.05. Relevant data from each included article, including the number of patients receiving antibiotic prophylaxis and in the control group, as well as the number of wound infections in each group, were input into the software. Different weights were assigned to each article based on the number of included patients. The choice between a random-effects model or fixed-effects model depends on the homogeneity of the articles. A fixed-effects model was applied when homogeneity was assumed, as it is suitable for small, similar studies. Use a random-effects model when expecting heterogeneity, suitable for diverse studies or unclear sources of variation.
The Egger’s test is a statistical test used to assess the presence of publication bias in a meta-analysis. It helps determine whether there is a systematic relationship between the effect size of individual studies and their standard errors, which could indicate the presence of bias in the literature.
Results
Study selection
In total, 1,122 records were identified through the initial literature search and after the manual reference list search. After removing duplicates and irrelevant articles, 181 records were screened for relevance. After the initial screening and exclusions, 112 records were assessed for full text assessment against the eligibility criteria. Finally, 11 records remained and were included after full-text assessment (Figure 1).
Study characteristics
Of the 11 records included, three were randomized clinical trials (RCT) (16-18) and eight were non-RCTs (nRCTs) (19-26). Eight studies evaluated dog bite data only (16-20,24-26), two evaluated mammalians (21,22), and one evaluated animals in general (23). A total of 852 patients with facial attacks were analyzed in this literature review (Table 1). The vast majority of facial attacks were dog bites (90.49%) but there were two articles (22,23) which mentioned bites from cats (six cases), rodents (three cases), horses (two cases), donkey (one case), and bird (one case). No study on human bites was included. Despite searching, no human bite article was added to this work. In another article, the number of bites divided by animals was ambiguous, despite a significant number of dog bites (91%) (21). No articles featuring wild animals, venomous animals, insects, and human attacks met the inclusion criteria. No clear predominance between gender and age group was found across articles. Seven articles were from the USA (16-19,22,25,26) and four from the European continent (20,21,23,24).
Table 1
| Reference | Origin | Type of study | N | Male/female | Mean age (years) | Animal/human | Most used antibiotic |
|---|---|---|---|---|---|---|---|
| Skurka et al., 1986 (16) | USA | RCT | 12 | NC | NC | Dog | Penicillin |
| Dire et al., 1992 (17) | USA | RCT | 70 | NC | 9.1 | Dog | Dicloxacillin |
| Quinn et al., 2010 (18) | USA | RCT | 94 | 55/39 | 32.53 | Dog | Amoxi-Clav |
| Callaham, 1980 (19) | USA | nRCT | 17 | NC | NC | Dog | Penicillin |
| Javaid et al., 1998 (20) | UK | nRCT | 40 | 17/23 | 25 | Dog | Amoxi-Clav |
| Wolff, 1998 (21) | Germany | nRCT | 68 | NC | NC | Mammalian | Penicillin |
| Kountakis et al., 1998 (22) | USA | nRCT | 29 | 18/11 | 12 | Mammalian | Amoxi-Clav |
| Kesting et al., 2006 (23) | Germany | nRCT | 132 | NC | NC | Animals | Amoxi-Clav |
| Zielińska-Kaźmierska et al., 2014 (24) | Poland | nRCT | 26 | 9/17 | 39.43 | Dog | Amoxi-Clav |
| Foster and Hudson, 2015 (25) | USA | nRCT | 20 | 9/11 | 20 | Dog | Ampicillin/sulbactam |
| Tabaka et al., 2015 (26) | USA | nRCT | 344 | 170/174 | 34.11 | Dog | NC |
RCT, randomized clinical trial; NC, not clear or not stated; Amoxi-Clav, amoxicillin and clavulanic acid; nRCT, non-randomized clinical trial.
Two articles concluded that maxillofacial bites should be treated with antibiotic prophylaxis (23,26). Two papers claimed that prophylaxis is only used in high-risk situations (18,19) while one contraindicated its use in low-risk wound infections (17). Three articles attested no benefit of using antibiotic prophylaxis in all cases given that the incidence of wound infections was similar in both groups (16,21,22). Amoxicillin + clavulanic acid (Amoxi-Clav) was the most commonly prescribed antibiotic prophylaxis in five articles (18,20,22-24).
Attacks on the face were less susceptible to wound infection than other anatomical regions, particularly the hands (16,19). Primary care seemed to be essential to prevent wound infection and for aesthetic and functional reasons (23). Five studies reported that this care was more important than the antibiotic prophylaxis (16,19-22).
Meta-analysis
A forest plot was created using RevMan 5.4 to evaluate the risk ratio of the included articles concerning the association between wound infection and antibiotic prophylaxis (Figure 2). The analysis indicated that the risk of wound infection was similar in both the antibiotic prophylaxis group and the control group, with a slightly higher but not statistically significant RD of 0.01 (95% CI: −0.02 to 0.05, P=0.40). The assessment of heterogeneity revealed moderate evidence of variability among the studies (P=0.05, I2=45%). To perform the meta-analysis, the fixed-effects model was employed.
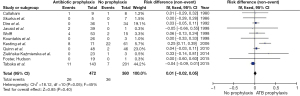
The risk of bias of the included articles was rated as high due to the lack of randomization (19-26) and blindness within the studies (Figure 3). Reporting bias was found in three articles (20,22,26). Some studies were at a high-risk of other biases due to non-use of most recommended antibiotics according to the literature (16,17,19,21).
A funnel plot was constructed to visualize the studies comparing antibiotic prophylaxis (Figure 4). It was observed that two studies (23,26) fell outside the boundaries of the funnel plot. This deviation can be attributed to the larger sample sizes in these studies compared to others. In order to further investigate the potential publication bias, Egger’s test was conducted, yielding a value of 5.2875 (95% CI: −10.6200 to 21.3276) with a significant P value of less than 0.0001. This significant asymmetry between studies indicates a high risk of bias in the publication of these studies. Egger’s test is a statistical analysis used to assess the presence of publication bias in research studies.
A list of excluded articles and their reasons was created (Table 2). These excluded articles were used for discussion but not for meta-analysis.
Table 2
| Reason for exclusion | Reference |
|---|---|
| (I) Animal studies | da Costa et al. (27) |
| (II) Antibiotic prophylaxis in all patients | Olaitan et al. (5), Paschos et al. (28), Kuvat et al. (29), Zangari et al. (30), Vitomir and Dragana (31), Donkor and Bankas (32), Gelvez et al. (33) |
| (III) Type of study | Chhabra et al. (34) |
| (IV) Not clear how many patients received antibiotic prophylaxis | Aloua et al. (8), Birdsey et al. (35), Piccart et al. (36), Chávez-Serna et al. (37), Kuhbier et al. (38), McGuire et al. (39), Nkomo et al. (40), Reuter Muñoz et al. (41), Sribnick et al. (42) |
| (V) Unclear about the affected anatomical region | Lang and Klassen (43), Brakenbury and Muwanga (44), Akhtar et al. (45), Changratanakorn et al. (46), Jones and Stanbridge (47) |
| (VI) Not found | Dahl (48), Monstrey et al. (49), Seijo et al. (50), Tomasetti et al. (51) |
Discussion
The increasing bacterial resistance observed in bacteria such as Streptococcus, E. coli, Pasteurella, Prevotella, and Bacteroides emphasizes the critical importance of avoiding the overuse of antibiotic prophylaxis (10,27). Overuse and misuse of antibiotics can lead to the emergence of resistant strains, rendering these medications ineffective in combating infections. Antibiotic resistance is a global public health concern that threatens our ability to effectively treat bacterial infections. By practicing appropriate antibiotic stewardship, healthcare professionals can help preserve the efficacy of antibiotics for future generations. This entails using antibiotics judiciously, only when necessary, and adhering to evidence-based guidelines for antibiotic prophylaxis. It is vital to weigh the potential benefits against the risks of antibiotic use, considering the individual patient’s condition and the specific circumstances of the procedure or injury. By adopting a multidisciplinary approach and working collaboratively, healthcare providers, researchers, policymakers, and the public can collectively address the challenge of antibiotic resistance and safeguard the effectiveness of these life-saving medications.
A preceding systematic review (4) concluded that antibiotic prophylaxis reduces the chance of contamination after human bites but not cat and dog bites. The same study confirmed that hand bite wound infections may be decreased when antibiotic prophylaxis is used. However, only two studies associated with the maxillofacial region were included (15,16). A richer blood supply to the head and neck might justify the decreased chance of wound contamination than in other anatomical regions (11,20,24,28).
Primary care for animal bite wounds is the cornerstone of preventing infection (29,30), and is superior to antibiotic prophylaxis (16,20). Wound irrigation with concerning 150–250 mL of saline with pressure is highly suggested (8,16,19-21,23-25). Punctures and deeper injuries are extra tough to irrigate (19,23). This explains why these types of wounds have a higher prevalence of infections. Cat bites additionally succeed a higher prevalence of infections for this reason, since cat teeth are thinner than other animal teeth (34). An antiseptic rinse after saline irrigation is considered crucial to lessen wound infections. A range of antiseptics may be used, including iodine-povidine (16,20) and hydrogen peroxide (23). Flushing with antibiotic solution has no evidenced benefit (25).
Delay in first attendance may be unfavorable (28,31-35). No delay pattern was found. Every study has established a unique lag time to suggest antibiotic prophylaxis, from 3 (21), 6 (22,23), 8 (24) to 24 hours (16,19).
The present study did not find evidence to indicate antibiotic prophylaxis in all instances of maxillofacial animal bites (95% CI: 0.01). Some studies indicate antibiotic prophylaxis in high-risk wound infections however not on low-risk conditions (16-19,21,26). Even for high-risk injuries, a few authors do not essentially advocate antibiotic prophylaxis, however instead conduct close follow-up (26). The extent appears not as crucial as the depth of the damage (17,21). Despite Lackmann’s (52) beneficial classification of bite wounds to the face and head by the severity, wound type was defined due to the fact few authors have used it (21,23). A summary of low- and high-risk of wound infections was provided (Table 3).
Table 3
| Features | Low risk (antibiotic prophylaxis no indicated) | High risk (antibiotic prophylaxis indicated) |
|---|---|---|
| Anatomical region | Face | Hand |
| Scalp | Foot | |
| Neck | ||
| Animal type | Dog | Cat |
| Birds | Monkey and other primates | |
| Rodents | Human | |
| Insects’ stings | Wild animals | |
| Unknown animal | ||
| Time of initial treatment | Right after trauma | Delayed |
| Wound type | Widest lesions | Puncture |
| Lacerations | Deep bites | |
| Abrasions | Contaminated bites | |
| Closed wounds | ||
| Health factors | – | Immunosuppressed |
| Diabetics | ||
| Advanced age | ||
| Alcoholism |
Due to the huge variety of animals microorganisms, there may be no particular antibiotic for all conditions (16). As the substantial majority of animal attacks are due to dog bites, approximately 80% to 90% (28,30,43), the foremost commonly prescribed antibiotic prophylaxis is Amoxi-Clav (18,20,22-24,37). The earlier use of penicillin has been replaced by Amoxi-Clav over the years. Useful towards a range of microorganisms typically found on bites, consisting of Streptococcus, E. coli, Pasteurella, Prevotella, and Bacteroides, in addition to Staphylococcus aureus (S. aureus) and Staphylococcus epidermidis (S. epidermidis) on the patient’s facial skin. There appear to be a disagreement concerning the number of days of antibiotic intake. Some authors required prophylaxis of wound infection for 3 days (16,18) and for others 5 to 7 days (19,23). Some authors advocate adding metronidazole to Amoxi-Clav for injuries caused by wildlife, humans and delayed initial treatment to manage anaerobic microorganisms (20,21). Patients with penicillin allergy ought to receive doxycycline (7) or azithromycin (23) as a second option.
Any person who has suffered an animal attack should have a history of tetanus vaccination. Animal bites, mainly wild and unknown are suspected to be related to tetanus and rabies (7). The equal applies to rabies prophylaxis particularly for cat, dog and wild animal bites. Contrary to the view of a few authors that antibiotic prophylaxis is much less vital for facial bites, rabies prophylaxis is more urgent because of the proximity to the central nervous system (43). Several alternative infectious diseases may be transmitted through bites such as Ebola, herpes, monkeypox, yellow fever, hepatitis B, human immunodeficiency virus (HIV), and tuberculosis (53).
One limitation of this study is the great difficulty of performing double-blind RCTs with statistical significance when investigating antibiotic prophylaxis in maxillofacial bite injuries (19). The included studies were not completely homogeneous (P=0.05, I2=45%), thus additional comparative studies with larger patient populations are desired to assess experimental and control groups and to achieve more evidence-based data and ideal doses. Secondly, relevant patient factors such as comorbidities, patient age, and wound factors (depth, tissue layers, size) were not assessed as they are not available in most of the included articles. And finally, due to a lack of protocol in antibiotic prophylaxis, it was not possible to evaluate the appropriate dose, route of administration, and duration of treatment in each situation. The authors suggest that multicenter studies worldwide ought to assist on this situation. Internet use and worldwide collaboration should be beneficial.
Conclusions
According to the available literature, this systematic review has demonstrated no definitive conclusion on whether or not antibiotic prophylaxis should be given or not to patients with animal bites (RD: 0.01). Antibiotic prophylaxis should be earned in high-risk cases. The cost-benefit of growing bacterial resistance needs to be appraised. Studies with a lower risk of bias are required on this topic.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-18/rc
Peer Review File: Available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-18/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-18/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sidrak D, Green J, Nawathe P, et al. Canine-to-Human Transmission of Mycoplasma canis in the Central Nervous System. J Pediatric Infect Dis Soc 2022;11:28-30. [Crossref] [PubMed]
- Ingram BM, Colosimo CM, Weaver JS, et al. Reconstruction After Grizzly Bear Attack in Wyoming. Am Surg 2023;89:2780-1. [Crossref] [PubMed]
- Parente G, Gargano T, Di Mitri M, et al. Consequences of COVID-19 Lockdown on Children and Their Pets: Dangerous Increase of Dog Bites among the Paediatric Population. Children (Basel) 2021;8:620. [Crossref] [PubMed]
- Medeiros I, Saconato H. Antibiotic prophylaxis for mammalian bites. Cochrane Database Syst Rev 2001;CD001738. [PubMed]
- Olaitan PB, Uduezue AO, Ugwueze GC, et al. Management of human bites of the face in Enugu, Nigeria. Afr Health Sci 2007;7:50-4. [PubMed]
- Chidzonga MM. Human bites of the face. A review of 22 cases. S Afr Med J 1998;88:150-2. [PubMed]
- Agarwal P, Dhiman A, Rashid N, et al. Head and neck injuries after leopard attack: Presentation and management. Chin J Traumatol 2021;24:389-93. [Crossref] [PubMed]
- Aloua R, Kerdoud O, Kaouani A, et al. Restorative management of human bite injuries to the face: Case series. Ann Med Surg (Lond) 2021;62:249-52. [Crossref] [PubMed]
- Knobel Freud H, López Colomés JL, Serrano Sáinz C, et al. Animal bites. Study of 606 cases. Rev Clin Esp 1997;197:560-3. [PubMed]
- Callaham M. Controversies in antibiotic choices for bite wounds. Ann Emerg Med 1988;17:1321-30. [Crossref] [PubMed]
- Guy RJ, Zook EG. Successful treatment of acute head and neck dog bite wounds without antibiotics. Ann Plast Surg 1986;17:45-8. [Crossref] [PubMed]
- Palmer J, Rees M. Dog bites of the face: a 15 year review. Br J Plast Surg 1983;36:315-8. [Crossref] [PubMed]
- Igoumenakis D, Gkinis G, Kostakis G, et al. Severe odontogenic infections: causes of spread and their management. Surg Infect (Larchmt) 2014;15:64-8. [Crossref] [PubMed]
- Rastenienė R, Pūrienė A, Aleksejūnienė J, et al. Odontogenic Maxillofacial Infections: A Ten-Year Retrospective Analysis. Surg Infect (Larchmt) 2015;16:305-12. [Crossref] [PubMed]
- Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 2021;372: [Crossref] [PubMed]
- Skurka J, Willert C, Yogev R. Wound infection following dog bite despite prophylactic penicillin. Infection 1986;14:134-5. [Crossref] [PubMed]
- Dire DJ, Hogan DE, Walker JS. Prophylactic oral antibiotics for low-risk dog bite wounds. Pediatr Emerg Care 1992;8:194-9. [Crossref] [PubMed]
- Quinn JV, McDermott D, Rossi J, et al. Randomized controlled trial of prophylactic antibiotics for dog bites with refined cost model. West J Emerg Med 2010;11:435-41. [PubMed]
- Callaham M. Prophylactic antibiotics in common dog bite wounds: a controlled study. Ann Emerg Med 1980;9:410-4. [Crossref] [PubMed]
- Javaid M, Feldberg L, Gipson M. Primary repair of dog bites to the face: 40 cases. J R Soc Med 1998;91:414-6. [Crossref] [PubMed]
- Wolff KD. Management of animal bite injuries of the face: experience with 94 patients. J Oral Maxillofac Surg 1998;56:838-43; discussion 843-4. [Crossref] [PubMed]
- Kountakis SE, Chamblee SA, Maillard AA, et al. Animal bites to the head and neck. Ear Nose Throat J 1998;77:216-20. [Crossref] [PubMed]
- Kesting MR, Hölzle F, Pox C, et al. Animal bite injuries to the head: 132 cases. Br J Oral Maxillofac Surg 2006;44:235-9. [Crossref] [PubMed]
- Zielińska-Kaźmierska B, Wieczerzak L, Kozioł A, et al. Damage of facial soft tissues as a result of being bitten by a dog. Pol Przegl Chir 2014;86:364-9. [Crossref] [PubMed]
- Foster MD, Hudson JW. Contemporary update on the treatment of dog bite: injuries to the oral and maxillofacial region. J Oral Maxillofac Surg 2015;73:935-42. [Crossref] [PubMed]
- Tabaka ME, Quinn JV, Kohn MA, et al. Predictors of infection from dog bite wounds: which patients may benefit from prophylactic antibiotics? Emerg Med J 2015;32:860-3. [Crossref] [PubMed]
- da Costa FVA, Spanamberg A, Araujo RP, et al. Feline sino-orbital fungal infection caused by Aspergillus and Scopulariopsis. Acta Sci Vet 2019;47:383.
- Paschos NK, Makris EA, Gantsos A, et al. Primary closure versus non-closure of dog bite wounds. a randomised controlled trial. Injury 2014;45:237-40. [Crossref] [PubMed]
- Kuvat SV, Bozkurt M, Kapi E, et al. Our treatment approaches in head-neck injuries caused by animal bites. J Craniofac Surg 2011;22:1507-10. [Crossref] [PubMed]
- Zangari A, Cerigioni E, Nino F, et al. Dog bite injuries in a tertiary care children's hospital: A seven-year review. Pediatr Int 2021;63:575-80. [Crossref] [PubMed]
- Vitomir K, Dragana P. Maxillofacial bite injuries treatment—20 years experience. Open Med 2014;9:461-7. [Crossref]
- Donkor P, Bankas DO. A study of primary closure of human bite injuries to the face. J Oral Maxillofac Surg 1997;55:479-81; discussion 481-2. [Crossref] [PubMed]
- Gelvez M, Enrique R, Gajos G, et al. Animal and human bite injuries: a 5-year retrospective study in a large urban public hospital in Venezuela. Oral Maxillofac Surg 2017;21:425-8. [Crossref] [PubMed]
- Chhabra S, Chhabra N, Gaba S. Maxillofacial injuries due to animal bites. J Maxillofac Oral Surg 2015;14:142-53. [Crossref] [PubMed]
- Birdsey M, Edwards G, Abetz J, et al. Bite wounds and antibiotic prescription among patients presenting to an Australian emergency department. Int Emerg Nurs 2016;27:42-5. [Crossref] [PubMed]
- Piccart F, Dormaar JT, Coropciuc R, et al. Dog Bite Injuries in the Head and Neck Region: A 20-Year Review. Craniomaxillofac Trauma Reconstr 2019;12:199-204. [Crossref] [PubMed]
- Chávez-Serna E, Andrade-Delgado L, Martínez-Wagner R, et al. Experience in the management of acute wounds by dog bite in a hospital of third level of plastic and reconstructive surgery in Mexico. Cir Cir 2019;87:528-39. [PubMed]
- Kuhbier MA, Könneker S, Dastagir K, et al. Animal bite injuries caused by domestic and wild animals: retrospective analysis and development of a prognostic score. Handchir Mikrochir Plast Chir 2020;52:96-106. [PubMed]
- McGuire C, Morzycki A, Simpson A, et al. Dog Bites in Children: A Descriptive Analysis. Plast Surg (Oakv) 2018;26:256-62. [Crossref] [PubMed]
- Nkomo M, Mahomed Z, Laher AE. An Audit of Patients with Dog-bite Wounds Presenting to a Tertiary Level Hospital Emergency Department in South Africa. Cureus 2020;12:e6558. [Crossref] [PubMed]
- Reuter Muñoz KD, Powell LE, Andersen ES, et al. Analysis of Pediatric Dog Bite Injuries at a Level 1 Trauma Center Over 10 Years. Ann Plast Surg 2021;86:S510-6. [Crossref] [PubMed]
- Sribnick EA, Sarda S, Sawvel MS, et al. Dog bite injuries in children: Clinical implications for head involvement. Trauma 2016;18:210-5. [Crossref]
- Lang ME, Klassen T. Dog bites in Canadian children: a five-year review of severity and emergency department management. CJEM 2005;7:309-14. [Crossref] [PubMed]
- Brakenbury PH, Muwanga C. A comparative double blind study of amoxycillin/clavulanate vs placebo in the prevention of infection after animal bites. Arch Emerg Med 1989;6:251-6. [Crossref] [PubMed]
- Akhtar N, Smith MJ, McKirdy S, et al. Surgical delay in the management of dog bite injuries in children, does it increase the risk of infection? J Plast Reconstr Aesthet Surg 2006;59:80-5. [Crossref] [PubMed]
- Changratanakorn C, Fasawang N, Chenthanakit B, et al. Effectiveness of antibiotic prophylaxis in patients with centipede stings: a randomized controlled trial. Clin Exp Emerg Med 2021;8:43-7. [Crossref] [PubMed]
- Jones DA, Stanbridge TN. A clinical trial using co-trimoxazole in an attempt to reduce wound infection rates in dog bite wounds. Postgrad Med J 1985;61:593-4. [Crossref] [PubMed]
- Dahl E. Animal bites at the casualty department of the Oslo City Council. Tidsskr Nor Laegeforen 1998;118:2614-7. [PubMed]
- Monstrey SJ, Eeckhout K, Matton G. Dog bites of the face. Ned Tijdschr Geneeskd 1987;131:1667-70. [PubMed]
- Seijo A, Monroig J, Romer C, et al. Clinical and epidemiological analysis of rat bites in Buenos Aires. Medicina (B Aires) 2009;69:259-64. [PubMed]
- Tomasetti BJ, Walker L, Gormley MB, et al. Human bites of the face. J Oral Surg 1979;37:565-8. [PubMed]
- Lackmann GM, Isselstein G, Töllner U, et al. Facial injuries caused by dog bites in childhood. Clinical staging, therapy and prevention. Monatsschr Kinderheilkd 1990;138:742-8. [PubMed]
- Jenkins GW, Isaac R, Mustafa S. Human bite injuries to the head and neck: current trends and management protocols in England and Wales. Oral Maxillofac Surg 2018;22:77-81. [Crossref] [PubMed]
Cite this article as: Grillo R, Brozoski MA, Moreira SB, da Silva YS, Borba AM, da Graça Naclério-Homem M. Antibiotic prophylaxis for animal inflicted maxillofacial injuries: a systematic review and meta-analysis. Front Oral Maxillofac Med 2024;6:32.




