
Management of oral-mandibular substance loss at the Owendo University Hospital Center
Highlight box
Key findings
• This study presents a confident approach to managing oral and mandibular substance loss.
• We report that the reference treatment is a two-stage reconstruction in order to improve patient follow-up and rehabilitation, which is slow but necessary. The results of treatment were favorable in most of our cases without complications.
What is known and what is new?
• Loss of substance in the mouth and mandible is a prevalent issue worldwide.
• Our manuscript provides a comprehensive overview of the current reconstruction techniques and their effectiveness, depending on the cause and extent of the loss. We assert that our research will be a valuable resource for those seeking to address this issue with confidence and expertise.
What is the implication, and what should change now?
• Improving surgical equipment is necessary. Encouraging staff communication about treatment methods is crucial. Our specialty must be publicized, even though we operate in a low-income country.
Introduction
Background
A loss of bucco-mandibular substance is a permanent loss of continuity of the tissues of the oral cavity and the mandible. It most often falls within the framework of multi-tissue loss of substance which concerns, among other things, the skin, the mucous membrane, the muscle and the bone (1).
Rationale and knowledge gap
They are frequent and most often secondary to surgical excision of a tumor, trauma, infection, osteoradionecrosis or a congenital mandibular or oral anomaly (2-4).
Key finding
Depending on their extent, they impact variably on masticatory, phonatory, swallowing functions and facial aesthetics (1,5). Therefore, they require a treatment that not only aims to restore bone continuity but also to enhance aesthetics, oral-mandibular function and provide an acceptable quality of life to the patient (6). This reconstruction uses various materials that can be living or inert. When it is alive this material is mainly bony or cutaneous-muscular. When it is inert it is endo prosthetic.
Objective
The aim of our study is to determine the management of oromandibular substance loss at the Owendo University Hospital Center. We present this article in accordance with the STROBE reporting checklist (available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-88/rc).
Methods
Study design
The study was conducted at the Stomatology and Maxillofacial Surgery Department of Owendo University Hospital Centre (CHUO), which is the reference centre for traumatology in Gabon and has been in operation since March 2016.
The survey data were collected using a survey form (see Appendix 1), hospital records, consultation and hospitalisation registers, and the operating theatre procedure register.
The degree of mandibular substance loss was classified according to the Cariou classification for mandibular substance loss and the Tessier classification for labial substance loss of congenital origin (7).
This was a retrospective, descriptive, analytical, single-center cross-sectional study, covering a period of 6 years from 1st March 2016 to 1st March 2022. Patients were selected based on their medical records indicating substance loss due to trauma, congenital conditions, or tumours. The survey form was completed using files of patients who were hospitalized and operated for malformation or acquired loss of substance of the oral-mandibular sphere.
All cases of oral-mandibular reconstruction were included, whatever the etiology, having been hospitalized in the department, and with a complete file. Patients with incomplete files and maxillary involvement were excluded. The studied variables were: (I) epidemiological aspect: hospital prevalence, sex, age, profession, etiologies; (II) clinical aspect: in particular the consultation time and the topography of the lesions, and morphological assessment (panoramic dental X-ray, CT of the facial area); (III) therapeutic aspect: treatment time, type of intervention, means of reconstruction, duration of hospitalization; the evolution and the operating cost. The functional and aesthetic results include the quality of oral nutrition, speech, mouth opening (normal >3 cm), aesthetic result, and the symmetry of the contours.
The losses of substances from the mandible were classified according to the Cariou classification (7):
- Type Aa: involves the symphyseal region;
- Type Ab: involves the entire anterior mandibular arch, from angle to angle;
- Type La: the horizontal ramus;
- Type Lb: the horizontal and ascending ramus;
- Type T: extends over one half of the mandible.
Statistical analysis
These data were reported in a Microsoft Office 2016 Excel file. The statistical analysis was carried out using IBM’s SPSS® statistic 20 software. Continuous data are presented as mean ± standard deviation. Categorical data are presented as percentages. The chi-squared bilateral test with the Monte Carlo method for theoretical numbers less than 5 was used to compare the proportions. The Kruskal-Wallis test was used to study the relationship between qualitative and quantitative variables. The difference was statistically significant when P<0.05.
Ethical considerations
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the Owendo University Hospital Center (No. 0074[2023], data 2023.4.10), informed consent of this retrospective analysis was waived.
Results
Epidemiological aspects
Over the study period, 27 cases met the inclusion criteria, out of a total of 1,075 patients admitted to the department, i.e., an annual average of 4.5 cases and a prevalence of 2.51% (Figure 1). In our series, 18 patients (66.7%) were male, and 9 patients (33.3%) were female, and the gender ratio was 2:1. The average age of our patients was 29±17.34 years and ranged from 0 to 67 years. Most patients were aged between 20 and 30 years old and accounted for 1/3 of the total. All socio-professional strata were represented. The group of pupils and students constituted the largest proportion, with a frequency of 40.7% (11/27), followed by the group of housewives and unemployed with 29.6% (8/27) (Table 1). They were largely dominated by tumor excision surgery (n=19, 70.4%), followed very far by traumatic causes which represented 18.5% (5/27), and malformative causes 11.1% (3/27).
Table 1
| Profession | Type of substance loss | Type of equipment | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aa | Ab | La | Lb | T | Total | Costal graft | Iliac graft | TOLV | Krenkel splint | Pedicled flap | Non-pedicled flap | Total | Percentage | ||
| Students | 3 | 1 | 1 | 5 | 2 | 1 | 5 | 3 | 11 | 40.7 | |||||
| Housekeeper and unemployed | 2 | 2 | 1 | 1 | 6 | 5 | 2 | 1 | 8 | 29.6 | |||||
| Employees | 1 | 1 | 1 | 3 | 1 | 2 | 1 | 4 | 14.8 | ||||||
| Retired | 1 | 1 | 2 | 1 | 1 | 2 | 7.4 | ||||||||
| Manuel workers | 1 | 1 | 2 | 1 | 1 | 2 | 7.4 | ||||||||
| Total | 5 (18.5%) | 2 (7.4%) | 4 (14.8%) | 3 (11.1%) | 4 (14.8%) | 18 | 8 (29.6%) | 2 (7.4%) | 1 (3.7%) | 7 (25.9%) | 7 (25.9%) | 2 (7.4%) | 27 | 100 | |
TOLV, microvascular free bone transfer.
Diagnostic aspects
In this study, 18 (67%) patients had mandibular involvement, 7 (26%) had lip involvement, 1 (4%) patient had involvement of the floor of the mouth, as well as the associated mandible, lips and floor. Twelve patients performed a dental panoramic, or 44.4% (12/27) of cases, 5 patients performed a CT scan of the facial area, or 18.5% (5/27) of cases, 18.5% (5/27) also performed a CT scan and a dental panoramic at the same time. Four patients did not perform imaging.
Lesions located at the level of the horizontal branch represented 7 (25.9%) of cases, followed by lesions at the parasymphyseal level in 4 (14.8%) patients, of the symphysis in 3 (11.1%) patients, bi-angular in 2 (7.4%) patients and hemi-mandibular and angular in respectively 1 (3.7%) patient.
According to the Cariou classification, type Aa was the most frequent, found in 5 (18.5%) cases, and type Ab only found in 2 (7.4%) cases (Table 1).
Therapeutic aspects
Oral-mandibular reconstruction was carried out at the same operating time for 17 patients, or 63.0% (17/27) of cases, and deferred in 37.0% (10/27) of cases with provisional placement of a space maintainer (Figure 2).

Two stages reconstruction was more frequently observed in patients aged 10–19 and 20–29 years (Figure 3).
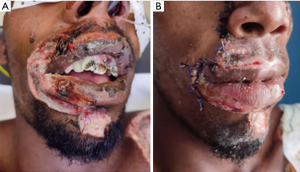
Ten patients with tumor-related substance loss benefited from a two-stage repair, i.e., 37% (10/27) of cases, and all loss of substance of traumatic origin benefited from a 1 stage reconstruction (Figure 4A,4B).
A revision for definitive repair was carried out in 37.0% (10/27) of cases; the average recovery time is 16.9 months; 59% (16/27) of the revisions were made after a period of 11 to 20 months, 30% (8/27) between 5 and 10 months, finally 10% (3/27) after a period of 20 months.
The use of bone grafts as a means of reconstruction was observed in 11 (40.7%) cases, followed by flaps in 9 (33.3%) patients. The rib graft was used in 8 (29.6%) patients, unlike the iliac graft which was used in 2 (7.4%) patients. The pedicled flap was used in 7 (25.9%) patients. The Krenkel splint is the only endoprosthesis that was used in 7 (25.9%) patients (Table 1).
Bone grafts and Krenkel splints had only been used for reconstruction of substance loss of tumor origin (Table 2). There was a relationship between the means of reconstruction and the etiology (P=0.001). Bone grafting was mainly used in female patients; while splints, pedicled and non-pedicled flaps have been used more in male patients (Table 2).
Table 2
| Means of reconstruction | Etiologies | Sex | Total | ||||
|---|---|---|---|---|---|---|---|
| Congenital | Traumatic | Tumoral | Male | Female | |||
| Rib graft | 0 | 0 | 8 | 3 | 5 | 8 | |
| Krenkel splint | 0 | 0 | 7 | 6 | 1 | 7 | |
| Pedicled flap | 3 | 4 | 0 | 5 | 2 | 7 | |
| Non-pedicled flap | 0 | 0 | 2 | 2 | 0 | 2 | |
| Iliac graft | 0 | 0 | 2 | 1 | 1 | 2 | |
| TOLV | 0 | 1 | 0 | 1 | 0 | 1 | |
| Total | 3 | 5 | 19 | 18 | 9 | 27 | |
TOLV, microvascular free bone transfer.
Evolution
The average follow-up duration is 22 days with extremes ranging from 7 to 480 days.
Two cases of surgical site infection were noted (7.4% of cases), treated by drainage and antibiotic therapy with good progress. The immediate postoperative course was simple for 85.2% (23/27) of our operated patients. We did not note any hemorrhage, hematoma, or complications of general anesthesia.
Two late complications (7.4%) were observed, notably a displacement of the osteosynthesis material and a floor fistula progressing towards death.
The postoperative course was complicated in 4 patients, 3 (11.1%) of whom had tumoral substance losses, and 1 (3.7%) patient of traumatic origin.
The postoperative course was simple in 16 patients who underwent 1-stage reconstruction and 7 patients who underwent 2-stage reconstruction. They were complicated in 3 (11.1%) patients who underwent 2-stage reconstruction, and 1 (3.7%) patient for 1-stage reconstruction.
The bone grafts were subject to two post-operative complications, notably a displacement of the osteosynthesis material and a secondary infection of the operating wound. The flaps were also subject to two complications, namely a floor fistula and a superinfection of the operating wound.
The diet was good in 14 (51.9%) patients; the patients’ speech results were satisfactory for 21 (77.8%) of patients; moderate limitation of mouth opening is observed in 7 (25.9%) patients; 23 (85.2%) of patients had a normal scar (Table 3).
Table 3
| Frequency (N=27) | Percentage | |
|---|---|---|
| Quality of oral nutrition | ||
| Good | 14 | 51.9 |
| Disturbed | 12 | 44.4 |
| Not specified | 1 | 3.7 |
| Speech | ||
| Normal | 21 | 77.8 |
| Moderatly impaired | 5 | 18.5 |
| Not specified | 1 | 3.7 |
| Mouth opening | ||
| Normal | 19 | 70.4 |
| Moderate limitation | 7 | 25.9 |
| Not specified | 1 | 3.7 |
| Aesthetic result | ||
| Normal scar | 23 | 85.2 |
| Hypertrophy | 1 | 3.7 |
| Unsightly scar | 1 | 3.7 |
| Not specified | 2 | 7.4 |
| Contour symmetry | ||
| Yes | 26 | 96.3 |
| No | 1 | 3.7 |
Discussion
Epidemiological aspects
Hospital prevalence
In six years, we have recorded 27 cases of oral-mandibular reconstructions, or an annual frequency of 4.5 cases. Furthermore, these reconstructions represent 2.51% of patients who visited the stomatology and maxillofacial surgery department during the study period.
Our annual frequency still remains low, and this could be explained by the fact that cases of maxillofacial trauma are under-reported and under-evaluated in our context. Not all patients entering the service have complete medical records. Also, some patients received treatment in other hospital structures and were not taken into account in our study. Therefore, the effort to systematically record all cases of consultation by all stakeholders is necessary.
Age
The young patients observed in this work, with an average age of 29 years, are reported by most African authors. Tagba et al. reported an average age of 34.5 years in Senegal (1), and Beogo et al. reported an average age of 26.6 years in Burkina-Faso (2). In studies from Western countries, a much higher average age is reported, which is 60 years according to David et al. (3) in France. In addition to the youth of the African population (4), this age difference between African and Western studies can be explained by the etiologies of substance loss. In the African series, they are dominated by excision surgery for benign tumors which is the prerogative of young subjects (2,5). In Western series, they are dominated by the excision of malignant tumors.
Sex
The observation of a male predominance (66.6%) compared to 33.3% of female patients is also reported by David et al. (3) in France. Amady et al. (6) as well as González-García et al. (8) in Spain also reported a male predominance with respective frequencies of 82.5% and 70.9%, which is not the case for the work of Tagba et al. (1) in Senegal and Ndukwe et al. (5) in Nigeria who reported a slight female predominance with 56.5% and 52%.
The profession
During our study we noticed that the majority of our patients were pupils and students in 40.7% of cases, followed by housewives and unemployed in 29.6% of cases. Our results are similar to those of Amady et al. in 2011, and those of Assouan et al. in 2014 who found that school and student patients were respectively the most affected by mandibular trauma in 35% of cases (6) and maxillofacial trauma in 63.3% of cases (9). Unemployment and the growing number of young unemployed graduates are causing an increase in violence and insecurity in our society. Kpemissi et al. found that this same professional group is mainly affected by loss of mandibular substances of tumor origin (10). This can be explained by the fact that disadvantaged groups are those most exposed to the etiologies of loss of oro-mandibular substances, which are benign tumors at an advanced stage.
Etiologies
Tumor excision surgery, representing the dominant etiology of substance loss in this study with 70.4% of cases, ameloblastoma in particular with 51.8% of cases, is reported by most African authors. This is how Beogo et al. (2) noted that 80% of substance losses are due to the excision of a benign tumor, of which 39.5% are attributable to ameloblastoma. Ndukwe et al. (5) reported 92% loss of substances due to surgery to excise benign tumors.
This state of affairs can be explained by the delay in consultation, which is common in Africa. Furthermore, ameloblastoma, the leading benign tumor, requires radical surgery due to its local aggressiveness and its high potential for recurrence. Oral-mandibular trauma takes second place with 18.5% of cases and all caused by a motor vehicle accident (MVA). Whatever the etiology, the male sex is the most affected. This second place is also highlighted by Ndukwe et al. with 4% of cases (5). In their 2012 study in Guinea Conakry (11), Diallo et al. found that 70.57% of maxillofacial trauma were caused by road accidents. This is due to the lack of road safety education, excessive speed, the non-use of safety helmets, the consumption of alcohol and psychoactive substances by the majority of drivers and, finally, the dilapidated and defective state of the road.
In Western studies, the authors report surgery and radiotherapy of cancers as the dominant etiologies of substance loss (3). These results, in opposite of ours, can be explained by the high life expectancy in the West, which has led to an increased incidence of carcinomas of the upper aero-digestive tracts, resulting in a rise in the use of surgeries and radiotherapy for cancers.
Diagnostic aspects
Topography
We noted a predominance of involvement of the mandible in 66.6% of cases followed by the lips in 25.9% of cases. Diallo et al. in 2012 (11) found that labial damage was almost superimposable to ours with 26.79% of cases. For Hussaini (12) this labial involvement predominates and concerns both lips with almost equal frequency, i.e., 22.8% for the upper lip and 18% for the lower lip. The frequency of lip involvement could be explained by greater exposure due to their prominence; they start from the bumper of the face. In addition, the region of the philtrum and lips is particularly vulnerable due to the presence of teeth which constitute a hard receiving plane during trauma.
Morphological assessment
Panoramic dental radiography is the most frequently used morphological examination, notably in 44.4% of our patients. Performing a CT scan is not systematic for a maxillomandibular tumor. However, in the case of an extensive lesion and/or suspected malignancy, a CT scan or even magnetic resonance imaging (MRI) could be conducted. It specifies the size and relationships of the tumor with neighboring elements. This will allow us to discuss operability and predict the limits of tumor resection (13).
Maxillofacial scanning was performed in five of our patients, i.e., 18.5%; but MRI was not performed in our series because of its accessibility and high cost. This is a known problem in our region.
Site of mandibular lesions
Tumor lesions, the cause of mandibular interruptive substance loss, can occur in all parts of the mandible, but the horizontal branch remains the most frequent location in this study with 25.9% of cases, followed by the para symphyseal region. These results are in agreement with those of Atallah et al. (14) who noted that the area of predilection is the horizontal branch with 28% of cases. Kpemissi et al. (10) found a predominance of lesions in the hemi-mandible in 48.35% of cases, followed by the horizontal branch in 19.78% of cases. Nitassi et al. (15) observed that the angular region represents the most frequent location, with an extension towards the horizontal branch in 70% of cases, followed by the parasymphyseal regions in 20% of cases and symphyseal in 10% of cases.
Therapeutic aspects
Operating times
1-step reconstruction
When the loss of oromandibular substance is created by the surgeon, reconstruction at the same time is always desirable. It is simpler and gives the best results. This is the usual situation for loss of mandibular interrupting substance linked to oncological resection. In the case of maxillo-mandibular trauma, the times must be shortened as much as possible because retractile healing occurs quickly on the soft tissues and, even if the bone fragments are held in place by fixators, this healing is detrimental to the final result. This reconstruction concerned 63.0% of our patients.
Reconstruction in 2 stages
This situation is encountered more and more frequently in oncology, sometimes out of habit, often justified by the pathological state of the patient. This situation is delicate and reconstruction is always difficult due to post-radio-surgical sclerosis; even if well carried out, brings little benefit.
In our series, the mandibular reconstruction was carried out at the same operating time for most cases, i.e., 63.0%, and delayed in 37.1% of cases with provisional placement of a space maintainer. This is consistent with data from the literature where immediate reconstruction was the most favored (16).
Repair materials
The reconstruction of oro-mandibular defects uses a variety of therapeutic means including flaps, bone grafts and metal splints. The bone graft is the material that is most used, notably in 40.7% of cases.
Means of reconstruction
The reconstruction of mandibular defects with a non-vascularized bone graft remains a pillar of mandibular reconstruction in Gabon. Microsurgical reconstruction of bucco-mandibular substance loss is the gold standard, although it remains difficult to perform in developing countries due to lack of technical resources. Although the use of nonvascularized grafts is largely limited in the reconstruction of large defects with or without soft tissue loss or in cases where adjuvant radiotherapy is indicated, the advantages of this option in restoring good esthetics and function facial in properly selected cases are well documented (17).
Resection of the mandible following tumor lesions is reported as the most common cause of mandibular substance loss requiring reconstruction. In this study, these defects were mainly reconstructed with bone grafts in 33.3% of cases. A recent report on oromandibular reconstruction agreed that nonvascularized grafts are best suited for the reconstruction of segmental defects resulting from the removal of benign lesions (18). However, Van Gemert et al. (18) reported a good measure of success with only 19% failure rate in the 27 patients reconstructed with a non-vascularized iliac crest graft.
For extensive mandibular interrupting substance defects, according to Kohen et al. (19), free flaps are more indicated than a conventional graft, which is more exposed to the risk of resorption and more susceptible to infections due to the proximity of the oral environment. Revascularized free flaps are, for their part, much more resistant to secondary infection and contamination by the oral environment and do not undergo resorption over time. In addition, their rich periosteal vascularization makes several modeling osteotomies possible, therefore a three-dimensional conformation of the flaps; which is a great aesthetic contribution. Unfortunately, accessibility to this process is limited by the low purchasing power of patients, despite universal health insurance. In fact, the vast majority of patients in our series belong to professional groups with low purchasing power.
All these reasons motivate the frequent choice of bone grafts, i.e., 33.3% of cases; iliac bone in 22.2% of cases and especially costal bone in 77.8% of cases for the reconstruction of the mandible (17). Also, to prevent the risk of failure of infectious origin, immediate reconstruction is preferably done using metal stents in 25.9% of patients; this choice of endoprosthesis is also motivated by the impossibility of carrying out an extemporaneous anatomo-pathological examination of the surgical specimen. In Gabon, the choice of the Krenkel metal splint is based on its greater accessibility, the large extent of the lesions and their rigidity.
Evaluation of results by the patient
The results in terms of patient satisfaction are measured according to several criteria including the quality of oral nutrition, speech, mouth opening, aesthetic result and symmetry of contours. In this study 51.9% of patients reported having a good diet; 77.8% of them found a voice that was intelligible to those around them; 25.9% noted a moderate limitation of mouth opening; the aesthetic result is acceptable in 85.2% of patients. Patients who were dissatisfied or disappointed with the surgical treatment did not expect the most modest functional results, but had unrealistic expectations, especially on the aesthetic level. Hence the need for clear and precise information for conscious patients or families before the intervention.
The study’s strength lies in its aim to inform us about the various causes of substance loss and the most effective means of reconstruction for its management.
However, the cost of treatment may mean that patients do not return for further treatment, and the shortage of surgeons in our region means that treatment options cannot be discussed.
Conclusions
Oral-mandibular substance loss mainly affects young, school-age male subjects. Their main etiology is surgery to excise tumors, particularly ameloblastoma; with the preferred site being the horizontal branch of the mandible. Panoramic dental radiography and maxillomandibular scanning highlight the loss of substance as well as its extent. The therapeutic choice is more often oriented towards a 2-stage oromandibular reconstruction using a splint and a costal bone graft. Definitive reconstruction through the rib gives us good morphological and aesthetic results and allows a soft diet to be introduced quickly.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-88/rc
Data Sharing Statement: Available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-88/dss
Peer Review File: Available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-88/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-23-88/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the Owendo University Hospital Center (No. 0074[2023], data 2023.4.10) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tagba E, Sy A, Ndiaye M. Diagnostic aspects and results of surgical treatment of maxillomandibular tumours: a case report about 23 Cases. J Afr Cancer 2014;6:228-34. [Crossref]
- Beogo R, Konsem T, Ouedraogo WF, et al. Repair of interrupting substance loss of the mandible by non vascularized bone grafting after ablative surgery for benign lesions at the Sourô Sanou University Hospital. bone graft after ablative surgery for benign lesions at CHU Sourô Sanou: Preliminary results. Rev Col Odonto-Stomatol Afr Chir Maxillofac 2010;17:30-4.
- David S, Dassonville O, Poissonnet G, et al. Failures in cervico-facial reconstructive surgery using free flaps: Favouring factors and management. Annals of Aesthetic Plastic Surgery 2011;56:308-14.
- Global statistics. Median age of the population in Africa and Europe. Available online: http://www.statistiques-mondiales.com/age_moyen_population.htm
- Ndukwe KC, Aregbesola SB, Ikem IC, et al. Reconstruction of mandibular defects using nonvascularized autogenous bone graft in nigerians. Niger J Surg 2014;20:87-91. [Crossref] [PubMed]
- Amady C, Ba B, Keita K, et al. Epidemiology of mandibular trauma treated at the CHU-CNOS in Bamako: 57 cases. African Journal of Dentistry and Implantology 2018;7:30-6.
- Cariou JL, Payement G, Rochebilière A, et al. Choice of free composite flap in the reconstruction of loss of substance in the mandible. Apropos of 28 cases. Ann Chir Plast Esthet 1994;39:449-60. [PubMed]
- González-García R, Naval-Gías L, Rodríguez-Campo FJ, et al. Reconstruction of oromandibular defects by vascularized free flaps: the radial forearm free flap and fibular free flap as major donor sites. J Oral Maxillofac Surg 2009;67:1473-7. [Crossref] [PubMed]
- Assouan C, Millogo M, Anzouan KE, et al. Maxillofacial Trauma at the Teaching Hospital of Treichville in Abidjan (Cote d’Ivoire). Epidemiologic Study of 1066 cases. Rev Col Odonto-Stomatol Afr Chir Maxillo-Fac 2014;21:31-4.
- Kpemissi E, Amana B, Tchandana K. Mandibular tumours: epidemology, diagnostic and therapeutic aspects concerning 91 cases. Mali Med 2009;24:47-52. [PubMed]
- Diallo OR, Camara SA, Diallo A, et al. Cervico-facial traumatic injuries at the Donka national hospital of the teaching hospital of Conakry. Mali Med 2012;27:1-5.
- Hussaini HM, Rahman NA, Rahman RA, et al. Maxillofacial trauma with emphasis on soft-tissue injuries in Malaysia. Int J Oral Maxillofac Surg 2007;36:797-801. [Crossref] [PubMed]
- Mejri I, Chelbi M, Daliet KM, et al. Radiohistological correlation in the diagnosis of radiolucent images maxillomandibular radiolucency: a case report of 120 patients. J Radiol 2005;86:1549. [Crossref]
- Atallah S, Bozec A, Ransy P, et al. Functional evaluation of mandibular reconstruction with bone free flap. A GETTEC study. Eur Ann Otorhinolaryngol Head Neck Dis 2021;138:82-8. [Crossref] [PubMed]
- Nitassi S, Boulaadass M, Tobi I, et al. Ameloblastoma: diagnosis and treatment. About 26 cases. Med Buccale Chir Buccale 2009;15:93-100. [Crossref]
- Alloh-Amichia. Mandibular reconstruction procedures in the Ivory Coast: problems encountered in 314 prosthesis. Rev Iv Odonto-Stomatol 2011;13:50-6.
- Harding B, Ouattara B, Koffi M, et al. Repair of loss of mandibular substance. Rev Iv Odonto-Stomatol 2005;7:6-9.
- van Gemert JT, van Es RJ, Van Cann EM, et al. Nonvascularized bone grafts for segmental reconstruction of the mandible--a reappraisal. J Oral Maxillofac Surg 2009;67:1446-52. [Crossref] [PubMed]
- El Kohen A, Benjelloun A, Benchekroun L, et al. Mandibular reconstruction: evolution of operative techniques. Report of 22 cases. Revue de Stomatologie et de Chirurgie Maxillo-faciale 2004;105:347-53. [Crossref] [PubMed]
Cite this article as: Makungu AP, Mikemou FNM, Foka RS. Management of oral-mandibular substance loss at the Owendo University Hospital Center. Front Oral Maxillofac Med 2025;7:1.



