
Can anxiety in third molar surgeries with different degrees of difficulty and extent interfere with the perception of postoperative pain and trismus?—An observational and prospective study
Introduction
The most widely accepted concept of anxiety in dentistry involves a complex pattern of behavior associated with a physiological activation that occurs due to an internal (cognitive and somatic) and an external (environmental) stimulus that patients can experience before and/or during treatment dental (1). Tooth extraction is a procedure commonly considered to be very stressful for patients and, among the extractions, third molars surgeries are the ones that may produce greater anxiety (1-6). In addition, patients with moderate to high anxiety may report more intense and prolonged pain during and after the surgical procedure, being also associated with spikes in blood pressure (BP) and heart rate (HR) (3,4,7-11) and, as a consequence, it may make the procedure more difficult to the surgeon (12).
A meta-analysis study developed by Astramskaitė et al. [2016] (7) observed that dental anxiety may be associated with patient’s own propensity to anxiety, previous experience or expectation of pain, discomfort during the procedure, marital status (single), social class (young students), type of local anesthesia applied (regional nerve block) and even, the method used by the surgeon to provide information about the surgery such as a video demonstration. However, according to the author, further studies are needed due to the occurrence of disagreements between the statements and observations.
The State-Trait Anxiety Inventory (STAI) has often been used to assess characteristics or levels of anxiety in patients undergoing dental surgery (1-7,13-15). This instrument can be used simultaneously to assess the patient’s trait and state of anxiety, with the trait being the characteristic of the individual’s subjective tendency to perceive the specific situation related to the stimulus or danger whereas, the state is defined as the subjective feeling of nervousness or a temporary state of stress and apprehension (4,14).
This study had the primary objective of verifying whether preoperative anxiety patterns in third molar surgeries (3Ms) with different degrees of difficulty and extension may interfere with the perception of pain and trismus postoperatively. Secondarily, the study sought to explore other characteristics that may be associated with the perception of anxiety, pain and trismus, such as surgical factors, drug prescription and systemic conditions. This article is in accordance with the STROBE reporting checklist (available at https://fomm.amegroups.org/article/view/10.21037/fomm-21-22/rc).
Methods
This study was classified as observational, cross-sectional, exploratory and prospective. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and it was submitted and approved by the University’s Ethical Committee for Human Research under the number 3.591.151 and a written informed consent was obtained from all study participants.
The inclusion criteria were patients seeking care and requiring surgery of third molars, nevertheless, with clear and defined indications for it, such as; for orthodontic indication, for prosthetic indication, associated pathology or even for prophylactic reasons, since the risks of the procedure does not exceed its benefits. Patients were included consecutively through a non-probabilistically model. As exclusion criteria, were removed patients with any medical condition that contraindicates dental surgical treatment, patients who did not consent or withdrew their consent, patients who presented postoperative complications such as infection, dry socket and any nerve paresthesia, as well as, those patients who did not return the postoperative diary or returned it with lack of answers or critical information.
Surgeries were done in dental setting and involved the removal of one or more third molars per procedure and classified as 1 upper third molar (G1), 1 lower third molar (G2) and two or more third molars (G3). All procedures were performed by oral and maxillofacial residents with the same degree of experience and, surgeries and postoperative evaluations were monitored and a postoperative diary were collected by two maxillofacial surgeons. Surgical procedures were performed under the strictest control of microbiological contaminants and included sterile surgical sheets, sterile drapes and sterile surgical gloves. All patients received prescriptions according to the resident and preceptor’s perspective and included analgesic, non-steroidal and/or prophylactic steroidal anti-inflammatory, antibiotics and prophylactic anxiolytics, however, the patient was allowed to suspend antalgic drugs if there were no symptoms, but they were instructed to take the medication as soon as the pain started, except for antibiotics where the patient should adhere to the recommended prescription. Mouthwash with 15 mL (milliliters) of 0.12% chlorhexidine solution was used before surgery.
Assessment of the difficulty of surgery
The difficulty of the surgery was obtained by a surgeon point-of-view through a verbal scale (0–5), considering the entire surgical process and obtained immediately after the end of the procedure using the following scale: [0] easy; [1] little difficulty; [2] medium difficulty; [3] great difficulty; [4] complex and; [5] very complex.
Assessment of the systemic condition
A modified American Society of Anesthesiologists Classification (ASA) physical classification system for dentistry was obtained through the questionnaire European Medical Risk Related History (EMRRH) (16). BP and HR were measured in a single opportunity, just before the start of the surgical procedure. These were collected through an automatic BP monitor was used (Omron Dalian Co., LTD, China, certified by the National Health Surveillance Agency at 8004730 * 0345). As a screening method a single-lead handheld portable electrocardiogram (ECG) PC-80-B was used (Food and Drug Administration approved: PC80B Easy ECG Monitor, Shangai Lishen Scientific Equipment Co., LTD, China). Each patient was submitted to, at least, two tests to confirm suspected alteration. Studies using a single-lead handheld ECG machines have reported that those devices are feasible to identify some cardiac diseases especially atrial fibrillation, with minimal training (17,18).
Pain assessment
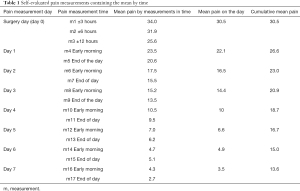
Patients received a diary and were instruct in how to fill it up for postoperative records. Pain was self-rated through a visual analogue scale (0–100) (19) and was obtained 17 times in the course of 8 days, starting at 3 hours after surgery (3 h, 6 h and 12 h to d 0), and at waking time and at the end of the day (standardized between 6 to 8 p.m.) for days 1 to 7. Patient should record pain considering the highest experience in the period between the previous annotations. The measurements were than transformed in the mean of the period (example: day 0 = mean of 3 measurements; 3, 6 and 12 hours after the surgery). In order to quantify the real amount of pain fent in the period, the pain scores were added consecutively and divided by the number of measurements creating the accumulated mean of pain (example: day 4 = mean of 11 measurements = accumulated mean of pain).
Trismus assessment
Trismus was assessed using a six-point ordinal, verbal and descriptive scale (0–5) according to the clinical situation observed by the patient, collected always at the end of the day, between day 0 to day 7; and for that, the following scale was used; [0] did not notice changes in the mouth opening; [1] noticed a small reduction in mouth opening; [2] mouth only opens about half the normal; [3] mouth only opens less than half the normal; [4] mouth opens almost nothing; [5] mouth is locked and cannot open anything.
Anxiety assessment (STAI)
The anxiety was scored through the STAI questionnaire which consists of 40 questions divided into two groups, which assess anxiety as a transient state (state anxiety) and latent trait (trait anxiety). State anxiety is considered a transitory emotional state, characterized by subjective feelings, apprehension, and autonomic nervous system hyperactivity. Trait anxiety identifies relatively stable individuals with a tendency to perceive situations as threatening. Both the state and trait scales consist of 20 items and both scales include direct and reverse-worded questions punctuations. The scores range from 20 to 80, with higher scores suggesting greater levels of anxiety (20). The STAI final scores were obtained through an online calculator (https://www.nsrusa.org/score.php) to avoid confusion about reversed worded punctuation for some questions or items.
Statistical procedures
A statistical program (IBM® SPSS® 15.0) was used to explore the data through descriptive and inferential analysis. A two-tailed probability P≤0.05 was regarded as statistically significant. The values were explored through the characteristics of the variable as continuous, ordinal or nominal with the statistical tests applied as recommended for those criteria. Postoperative complications and diaries with lacking critical data were excluded.
Results
Patients and systemic conditions
The sample consisted of 68 patients aged between 18 and 43 years (mean 22±4). The majority of the sample was composed of females (45 patients; 66.2%). Forty patients (58.8%) were attending university, while 12 (17.6%) patients had completed university education. The sample characteristics showed that most patients were ASA I and II, with only 2 patients classified as ASA III, these being; one patient with decompensated hypothyroidism, and one patient with a history of severe allergic reaction with history of previous hospitalization. Two patients were smokers (2.9%) with an average consumption of 5 cigarettes a day. The analysis by portable EEG revealed 5 patients with abnormalities, all of which were related to the increase in HR above 100 beats per minute (bpm), while the sample mean were 82 beats per minute (bpm). The mean systolic BP was 118 mmHg while the mean diastolic was 78 mmHg.
Surgical procedure
This sample does not include patients with postoperative complications such as paresthesia, infection and dry socket. The extractions were as follows: G1, 20 procedures; G2, 15 procedures and; G3, 33 procedures. The sample mean of the surgical time was 60 minutes and the average amount of anesthetic used was approximately 3 tubes (of 1.8 mL).
The surgical difficulty as described by the surgeon were as follows: 25 (36.8%) procedures were considered easy, 19 (27.9%) little difficulty, 14 (20.6%) medium difficulty, while procedures of great difficulty to very complex added up 12 procedures (14.7%). Antibiotics were used in 42.6% of the procedures, non-steroidal anti-inflammatory drugs in 91.2%, analgesics were used in 76.5%, a prophylactic single dose of corticosteroid in 8.8% and a prophylactic single dose of anxiolytic was used in 10 patients (14.7%). The 17 measurements in the 8-day course of pain and trismus are described in Tables 1 and 2, respectively. The STAI-State ranged from 22 to 62 points (35±8.4), while the STAI-Trait ranged between 23 to 62 points (37±7.7).
Full table

Full table
Systemic condition and anxiety
Anxiety did not differ significantly between patients age, gender and health status (ASA), however, the means of State-STAI anxiety scores were higher in patients classified as ASA II or superior (ASA I, 34.9 versus ASA II or higher, 37.7). The STAI scores showed no association with HR and BP. The handheld EEG device was able to detect abnormality and all abnormal cases were related with increased HR (normal ECG result, mean of 80 bpm; abnormal ECG result, mean of 107 bpm; t-test; P<0.001).
Anxiety, surgery and postoperative
The amount of pain did not vary significantly between groups in repeated measures analysis considering 8 measurements of pain, from day zero to day seven (ANOVA for repeated measurements, P>0.5). It is noteworthy that there was no significant variation between the groups concerning analgesic usage (ANOVA, P=0.74), anti-inflammatory (ANOVA, P=0.27) and corticosteroids (ANOVA, P=0.37). However, regarding the use of antibiotics, there was a greater use of this drug class for G3 when compared with the both remaining groups (ANOVA, Tukey HSD, P<0.001). The G3 also had longer surgical time necessary to complete the procedure (ANOVA, Tukey P=0.001) and higher anesthetics consumption (ANOVA, Tukey P<0.001) when compared with the both remaining groups. The length of the procedure did not show any correlation with the pain averages according to the period of evaluation, from day 0 to day 7, however, it (length) showed a correlation with the amount of anesthetic used (Pearson’s Correlation Test, P<0.001). The amount of anesthetic, in turn, also did not show associations with pain averages according to the day of assessment.
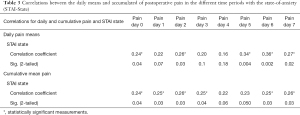
Postoperative pain showed correlations with greater scores of state-of-anxiety (STAI-State) both when analyzing the mean daily pain, and when analyzed with the mean accumulated pain, however, no correlations were observed with trait-anxiety (STAI-Trace) (Table 3). The anxiety (STAI) did not vary according to the surgical groups, did not influence the trismus self-perception, and did not interfere with the surgeon’s perception of surgical difficulty. The accumulated mean pain showed positive and statistically significant associations with the reduction of mouth opening on all assessment days (mean accumulated pain versus trismus, day-to-day assessment, Spearman’s correlation test, d0, P<0.001; d1, P<0.001; d2, P=0.002; d3, P=0.001; d4, P<0.001, d5, P<0.001; d6, P=0.001 and; d7, P=0.04), while mean daily pain showed positive and significant associations with reduced mouth opening until the fifth day of assessment (mean daily pain versus trismus, day-to-day assessment, Spearman’s correlation test, d0, P<0.001; d1, P=0.002; d2, P=0.001; d3, P=0.001; d4, P=0.002, d5, P=0.003; d6 and d7, non-significant associations found). Trismus showed significant associations with longer procedures up to the fourth postoperative day (Spearman’s correlation test, d0, P=0.002; d1, P=0.002; d2, P=0.001; d3, P<0.001; d4, P=0.02).
Full table
The prophylactic prescription of anxiolytics was correctly used for patients who had higher scores of state-of-anxiety (STAI-State) (prophylactic anxiolytic were not used in 58 patients, STAI-State mean was 34.2; used prophylactic anxiolytic were used in 10 patients, STAI-State mean was 43.5; t test, P=0.001). The use of prophylactic anxiolytics did not influence the daily mean and accumulated indexes of postoperative pain, trismus or the operator’s report of difficult surgery. The use of corticosteroids in a single prophylactic dose also did not show statistically significant differences for pain and trismus ratings. Antibiotic use prevented higher rates of trismus until day 3 (Mann-Whitney, respectively: d0 P=0.005; d1 P=0.008; d2 P=0.02; d3 P=0.04).
The surgeon’s characterization of the surgery difficulty may be indicative for the development of trismus up to the 3rd postoperative day (Pearson’s correlation: d0 r=0.4, P=0.001; d1, r=0.41, P<0.001; d2, r=0.35, P=0.005; d3, r=0.38, P=0.002), however, the difficulty of the surgery did not show a consistent association with postoperative pain.
Discussion
Third molar extraction is one of the most common invasive procedures in dentistry (21) and, in these procedures, patients may experience discomfort, restriction in daily activities and, in addition, patients may experience postoperative complications such as pain and trismus, among others (22,23). In this observational and prospective clinical trial, it was sought to know the effect and interaction produced by dental anxiety in postoperative pain and trismus following 3Ms extractions with different degrees of difficulty and extension, giving to this study a clear differential, since standardization with similar procedures has been the rule in this type evaluation in the current literature. It also brings a wide range of influencing variables, allowing us to have a broad view of such factor’s interactions providing to the dentist a close perspective of real life. This study also sought to investigate and explore the associations between these wide range of variables in order to better understand the effects and modulations of these factors on the most common complaints related to the postoperative period.
Anxiety in dental treatment is common and has been defined as an organic response characterized by apprehension and increased vigilance in situations of uncertainty, danger or potential threats to the integrity of the organism (9). The etiology of this anxiety is multifactorial, it can be caused by individual internal characteristics, it may be related to the procedure itself, or even influenced by previous negative experiences in addition to other factors not clearly evident (1-6).
It has been reported that 3Ms extractions may be significantly more difficult in anxious patients, and this status may also imply in physiological effects such as increased HR and BP (5,8,12). Still, in this context, dental anxiety can be a significant predictor of pain during and after dental treatment (4,9-11). Lin et al. (9) notes that anxiety should be understood as a fundamental step not only for the management of the condition, but also for better pain control in surgical procedures and, understanding these aspects, better controlling this emotional state can mean comfort for both patient and dentist (7). The results of the present study are in agreement with previous studies that indicate that high levels of anxiety are associated with higher pain indices reported after surgical dental treatment (9,10), however, the results also indicate that this increase of the postoperative anxiety-related pain is independent of the number of third molars extracted in a single procedure, a finding that should be highlighted as unprecedented in current literature. Another observation was that the prophylactic prescription of a single dose of anxiolytic does not seem to provide a beneficial effect on postoperative pain, however, new studies with improvements in the dosage and extension of use of this class of drugs may be useful for better pain management, especially about the pain which has an underlying anxiety profile.
Trismus or mouth opening limitation, another variable studied in the present clinical trial, is a common complaint after the 3M extractions. Since postoperative pain has been associated with anxiety states, it is plausible to accept the hypothesis that anxiety may have an effect on the perception of trismus as well. The findings of the present study did not confirm this eventual statement, although pain was strongly associated with this condition (trismus), especially until the fifth postoperative day (day 5). Trismus has been associated with extractions of 3Ms, as well as, surgical time and complexity of the procedure and also with development of infection and dry socket (22,23). The current study corroborates the findings in the literature regarding association between trismus and the length of the procedure, as well as, observes that the operator’s perception of the surgery complexity is also associated with a greater reduction in mouth opening.
This prospective clinical trial brought a large number of variables and data in order to better understand the process and the interaction of postoperative pain and trismus with different extension of 3M surgeries and anxiety. It should also be noted that this range of factors that are not controlled purposefully, may reflect the real life of the dentists and give then a piece of understanding to better deal and treat patients, however, due to the nature of observational studies, the answers to the hypothesis stablished here should still be viewed with prudence, understanding the nature of such kind of research.
Conclusions
Within the limitations of this study, it was possible to observe that postoperative pain showed correlations with the high levels of state-anxiety (STAI-state) regardless of the amount of third molars removed in a single procedure, however, no correlations were observed with the trait-anxiety (STAI-trait). Anxiety did not influence the patient’s perception of trismus. According to surgical prescription, it could be observed that the use of antibiotics prevented higher rates of trismus until the third postoperative day. Anxiolytics were more frequently prescribed for patients who had higher levels of anxiety, but did not influence the postoperative pain and trismus. The use of corticosteroids in a single prophylactic dose did not produce clear benefits. Surgical difficulty showed to be associated with the high indices of trismus, but did not show a consistent association with postoperative pain.
Acknowledgments
We want to thank the Brazilian National Council for Scientific and Technological Development (CNPq, Portuguese: Conselho Nacional de Desenvolvimento Científico e Tecnológico), Brazil, for the scholarship granted to Izabelle Millene Semczik, undergraduate student, as research assistant.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://fomm.amegroups.org/article/view/10.21037/fomm-21-22/rc
Data Sharing Statement: Available at https://fomm.amegroups.org/article/view/10.21037/fomm-21-22/dss
Peer Review File: Available at https://fomm.amegroups.org/article/view/10.21037/fomm-21-22/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.org/article/view/10.21037/fomm-21-22/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was submitted and approved by the University’s Ethical Committee for Human Research under the number 3.591.151 and informed consent was obtained from all study participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- López-Jornet P, Camacho-Alonso F, Sanchez-Siles M. Assessment of general pre and postoperative anxiety in patients undergoing tooth extraction: a prospective study. Br J Oral Maxillofac Surg 2014;52:18-23. [Crossref] [PubMed]
- Tarazona B, Tarazona-Álvarez P, Peñarrocha-Oltra D, et al. Anxiety before extraction of impacted lower third molars. Med Oral Patol Oral Cir Bucal 2015;20:e246-50. [Crossref] [PubMed]
- Wang TF, Wu YT, Tseng CF, et al. Associations between dental anxiety and postoperative pain following extraction of horizontally impacted wisdom teeth: A prospective observational study. Medicine (Baltimore) 2017;96:e8665 [Crossref] [PubMed]
- Reyes-Gilabert E, Luque-Romero LG, Bejarano-Avila G, et al. Assessment of pre and postoperative anxiety in patients undergoing ambulatory oral surgery in primary care. Med Oral Patol Oral Cir Bucal 2017;22:e716-22. [Crossref] [PubMed]
- Le SH, Tonami K, Umemori S, et al. The potential of heart rate variability for exploring dental anxiety in mandibular third molar surgery. Int J Oral Maxillofac Surg 2018;47:809-15. [Crossref] [PubMed]
- Yamashita K, Kibe T, Ohno S, et al. The Effects of Music Listening During Extraction of the Impacted Mandibular Third Molar on the Autonomic Nervous System and Psychological State. J Oral Maxillofac Surg 2019;77:1153.e1-8. [Crossref] [PubMed]
- Astramskaitė I, Poškevičius L, Juodžbalys G. Factors determining tooth extraction anxiety and fear in adult dental patients: a systematic review. Int J Oral Maxillofac Surg 2016;45:1630-43. [Crossref] [PubMed]
- Hollander MH, Schortinghuis J, Vissink A. Changes in heart rate during third molar surgery. Int J Oral Maxillofac Surg 2016;45:1652-7. [Crossref] [PubMed]
- Lin CS, Wu SY, Yi CA. Association between Anxiety and Pain in Dental Treatment: A Systematic Review and Meta-analysis. J Dent Res 2017;96:153-62. [Crossref] [PubMed]
- Heaton LJ. Self-reported Dental Anxiety is Associated With Both State Anxiety and Dental Procedure-Related Pain. J Evid Based Dent Pract 2017;17:45-7. [Crossref] [PubMed]
- Lago-Méndez L, Diniz-Freitas M, Senra-Rivera C, et al. Postoperative recovery after removal of a lower third molar: role of trait and dental anxiety. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:855-60. [Crossref] [PubMed]
- Aznar-Arasa L, Figueiredo R, Valmaseda-Castellón E, et al. Patient anxiety and surgical difficulty in impacted lower third molar extractions: a prospective cohort study. Int J Oral Maxillofac Surg 2014;43:1131-6. [Crossref] [PubMed]
- Doganer YC, Aydogan U, Yesil HU, et al. Does the trait anxiety affect the dental fear? Braz Oral Res 2017;31:e36 [Crossref] [PubMed]
- Koga S, Seto M, Moriyama S, et al. Anxiety before dental surgery under local anesthesia: reducing the items on state anxiety in the State-Trait Anxiety Inventory-form X. J Dent Anesth Pain Med 2017;17:183-90. [Crossref] [PubMed]
- Leal PC, Goes TC, da Silva LCF, et al. Trait vs. state anxiety in different threatening situations. Trends Psychiatry Psychother 2017;39:147-57. [Crossref] [PubMed]
- Abraham-Inpijn L, Russell G, Abraham DA, et al. A patient-administered Medical Risk Related History questionnaire (EMRRH) for use in 10 European countries (multicenter trial). Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:597-605. [Crossref] [PubMed]
- Grubb NR, Elder D, Broadhurst P, et al. Atrial fibrillation case finding in over 65 s with cardiovascular risk factors - Results of initial Scottish clinical experience. Int J Cardiol 2019;288:94-9. [Crossref] [PubMed]
- Proietti M, Farcomeni A, Goethals P, et al. Cost-effectiveness and screening performance of ECG handheld machine in a population screening programme: The Belgian Heart Rhythm Week screening programme. Eur J Prev Cardiol 2019;26:964-72. [Crossref] [PubMed]
- Bortoluzzi MC, Capella DL, Barbieri T, et al. A single dose of amoxicillin and dexamethasone for prevention of postoperative complications in third molar surgery: a randomized, double-blind, placebo controlled clinical trial. J Clin Med Res 2013;5:26-33. [Crossref] [PubMed]
- Spielberger CD, Gorsuch RL, Lushene RD. STAI: manual for the State – Trait Anxiety Invetory. Palo Alto, CA: Consulting Psychologists Press, 1970.
- Kim Y, Kim S, Myoung H. Independent predictors of satisfaction in impacted third molar surgery patients. Community Dent Oral Epidemiol 2010;38:274-86. [Crossref] [PubMed]
- Passarelli PC, Rella E, Piccirillo GB, et al. How frequent are postoperative complications after an impacted mandibular third molar extraction? J Biol Regul Homeost Agents 2020;34:1209-11. [PubMed]
- Hounsome J, Pilkington G, Mahon J, et al. Prophylactic removal of impacted mandibular third molars: a systematic review and economic evaluation. Health Technol Assess 2020;24:1-116. [Crossref] [PubMed]
Cite this article as: Gonçalves RCG, Jabur RO, Faria KW, Semczik IM, Gross DJ, Bortoluzzi MC. Can anxiety in third molar surgeries with different degrees of difficulty and extent interfere with the perception of postoperative pain and trismus?—An observational and prospective study. Front Oral Maxillofac Med 2021;3:25.

